Clinical guidance on evaluation and management of cardiogenic shock: A pragmatic, evidence-based roadmap from the American College of Cardiology
EDITORIALS
Clinical guidance on evaluation and management of cardiogenic shock: A pragmatic, evidence-based roadmap from the American College of Cardiology
Article Summary
- DOI: 10.24969/hvt.2025.567
- CARDIOVASCULAR DISEASES
- Published: 22/05/2025
- Received: 20/05/2025
- Accepted: 20/05/2025
- Views: 9054
- Downloads: 2300
- Keywords: editorial
Address for Correspondence: Gabriele Martelli, Azienda Ospedale – Università di Padova, Via Nicolò Giustiniani, 2, 35128 Padua, Italy
E-mail: gabriele.martelli@aopd.veneto.it
Gabriele Martelli , Ivo Tiberio
Intensive Care Unit U.O.C. Anesthesia and Reanimation, Department of Surgery, Padua University Hospital, Padua, Italy
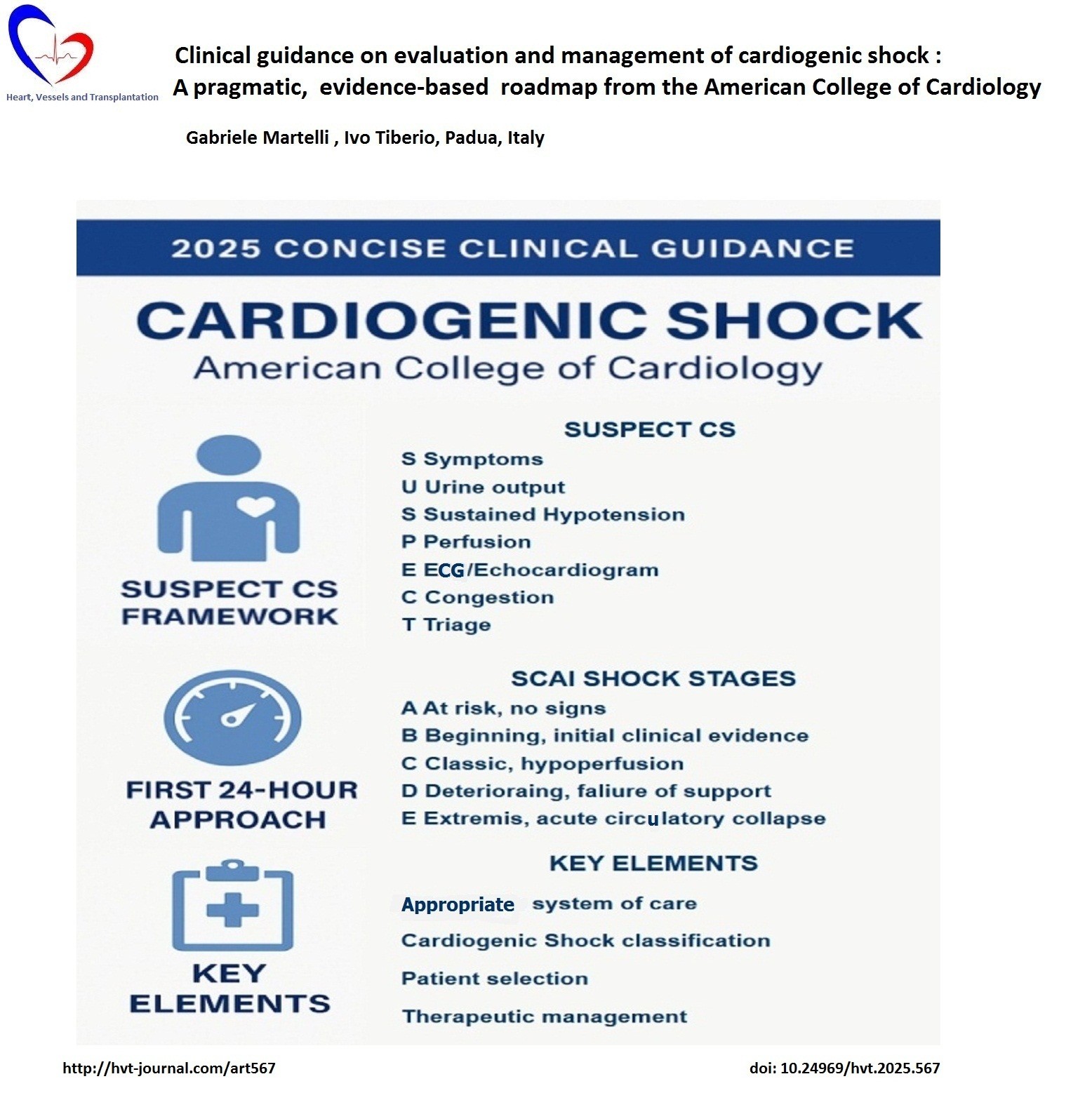
Graphical abstract
Cardiogenic shock remains a complex syndrome characterized by significant morbidity and mortality, despite the advancement in therapeutic interventions (1).
The American College of Cardiology's (ACC) document “2025 Concise Clinical Guidance: An ACC Expert Consensus Statement on the Evaluation and Management of Cardiogenic Shock” (2) introduces a structured, evidence-based approach to assist the physician in the management of cardiogenic shock.
The Concise Clinical Guidance represents a novel clinical format, designed to be focused and limited in scope. This approach is relevant to cardiogenic shock, a dynamic, multi-organ syndrome demanding rapid, coordinated, and evidence-informed care.
The document introduces some new issues on the initial assessment and classification of cardiogenic shock. The authors focused on the implementation of "SUSPECT CS" mnemonic, a tool designed for the early assessment, determined by clinical signs of congestion and hypoperfusion, alongside instrumental exams. The diagnostic evaluations, including electrocardiography and echocardiography, are emphasized to confirm the diagnosis and guide initial management.
Regarding the classification of shock, the Consensus Statement endorses the Society for Cardiovascular Angiography and Interventions (SCAI) five-stage classification system (3), which provides a lexicon to describe the evolving severity of shock (From “at risk” Stage A to “extremis” Stage E). This stratification has quickly gained traction in both academic and community settings due to its simplicity and clinical utility. Notably, the authors advocate for serial SCAI staging within the first hours of shock recognition, a critical period where the trajectory of disease and response to therapy are most malleable. This type of assessment encourages a proactive rather than reactive posture in shock management.
Treatment of cardiogenic shock has traditionally been dichotomized into pharmacologic support and mechanical circulatory interventions.
The 2025 ACC guidance offers a more integrated model, moving beyond previous paradigms to advocate for tiered, physiology-driven escalation of support. While acknowledging the continued role of pharmacological agents such as inotrope and vasopressors, the authors maintain a cautious stance in their endorsement, noting that these pharmacological agents remain a double-edged sword: they provide improvement at the cost of increased detrimental effects if not titrated correctly.
Furthermore, it is indicated to base the selection on the pathophysiological mechanism of the selected drug, as there is no evidence in the literature to support the superiority of a particular drug (4). The document endorses early consideration of mechanical support. Unlike previous statements, which tended toward permissive ambiguity, the 2025 guidance advocates for a structured algorithmic approach to mechanical circulatory support selection tailored to the phenotypic presentation of cardiogenic shock. The DanGer Shock trial (5) marks a pivotal moment in support of this view. In this large, randomized trial comparing early microaxial flow pump Impella CP insertion to conventional therapy in patients with CS, the primary outcome of 180 day all-cause mortality was significantly reduced in the mechanical support group. This represents one of the first high-quality demonstrations of a survival advantage with mechanical support devices and is redefining current practice.
On the other side of the therapeutic intervention, the authors framed the concept of de-escalation. De-escalation is a domain often overshadowed by the urgency of device initiation. Liberation from support is not merely a technical feat but a therapeutic milestone. Protocolized weaning strategies and pre-determined endpoints are necessary not just to optimize outcomes but also to minimize iatrogenic harm. This represents an improvement in the field’s philosophy: supporting life is not synonymous whit prolonging dying.
Critical care management of cardiogenic shock is covered in detail in the document. These management is regarded not passive maintenance but an active and evolving process of clinical improvement through hemodynamic optimization, multiorgan support, and structured assessment.
The use of invasive hemodynamic monitoring is central. Although randomized data are sparse, robust observational evidence supports an invasive approach to categorize the cardiogenic shock phenotype, to tailor therapy and guide the timing of mechanical support escalation or weaning (6).
This is particularly important in the early phase of shock, where a complete assessment of the hemodynamic profile has been shown to significantly reduce mortality compared with no or incomplete hemodynamic assessment (7).
Moreover, the 2025 guidance recommends structured, protocolized reassessment of clinical, imaging, and hemodynamic parameters. This approach not only informs therapeutic efficacy but also aids in recognizing the trajectory of recovery or decline.
Perhaps the most consequential aspect of the 2025 guidance is its systemic vision. Cardiogenic shock is no longer conceptualized as a problem solvable by a single physician or even a single institution. Rather, it is framed as a systems emergency, requiring vertically integrated networks of care, akin to existing paradigms in STEMI and stroke management.
The document suggests a three-tiered systemic model, where the most advanced level center (level 1) provides the highest standards of care available, is able to treat all types of cardiogenic shock, and serves as a consultant for secondary centers and case selection. Several observational studies (8), have demonstrated the mortality benefit of care in dedicated shock centers.
Additionally, shock teams, comprising cardiologists, intensivists, surgeons, perfusionists, and nurses, are enshrined as standard of care. This codifies what many leading centers have already practiced for years: that collective decision-making trumps hierarchical inertia (9). Moreover the guidance emphasizes that these teams must be empowered, not just appointed. Institutional commitment must extend beyond policy into real-time operational authority.
The 2025 ACC Concise Clinical Guidance on cardiogenic shock is not merely a clinical document but it is a manifesto for a new standard of care.
By anchoring its recommendations in evidence, operational feasibility, and ethical clarity, it provides a roadmap for both frontline clinicians and health system architects.
There is, of course, more work to be done. Randomized trials on treatment strategies remain scant, long-term outcomes poorly defined, and global implementation deeply uneven. But this guidance provides a foundation on which such work can be built. It is now incumbent upon institutions, payers, and policy-makers to align their structures with the recommendations herein.
Cardiogenic shock may never be “solved.”, but with documents like this, we move closer to managing it with the efficacy, responsiveness, and humanity that our patients deserve.
Peer-review- Internal
Conflict of interest- None to declare
Authorship: G.M. and I.T. equally contributed to in manuscript preparation and fulfilled authorship criteria.
Acknowledgement and Funding: None to declare
Statement on A.I.-assisted technologies use- Authors declare that they did not use AI-assisted technologies in preparation of this manuscript
Availability of data and material: Do not apply
References
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

