Comparative outcomes of retropubic versus transvesical open adenomectomy in benign prostatic hyperplasia: A retrospective cohort study
ORIGINAL RESEARCH ARTICLE
Comparative outcomes of retropubic versus transvesical open adenomectomy in benign prostatic hyperplasia: A retrospective cohort study
Article Summary
- DOI: 10.24969/hvt.2025.580
- CARDIOVASCULAR DISEASES
- Published: 22/07/2025
- Received: 20/04/2025
- Revised: 03/07/2025
- Accepted: 03/07/2025
- Views: 3029
- Downloads: 1403
- Keywords: Benign prostatic hyperplasia, retropubic adenomectomy, bleeding, postoperative hemoglobin drop, length of hospital stay, lower urinary tract symptoms
Address for Correspondence: Damirbek Abibillaev, Faculty of Medicine, Ala-Too International University, Bishkek, Kyrgyzstan
Email: damirbek.abibillaev@alatoo.edu.kg
ORCID: Abduzhalal Baktybek Uulu - 0009-0002-5213-8824, Akylbek Usupbaev - ORCID 0000-0003-1926-384X, Beksultan Ismatov - 0000-0003-1926-384X, Damirbek Abibillaev - 0000-0002-4660-3064, Bekmurza Konurbaev- ORCID 0009-0000-8103-1367
Abduzhalal Baktybek Uulu1,2, Akylbek Usupbaev2,3, Beksultan Ismatov2,3, Damirbek Abibillaev4, Bekmurza Konurbaev4
1 Department of Urology, S.B. Daniyarov Kyrgyz State Medical Institute of Postgraduate Training and Continuous Education, Bishkek, Kyrgyzstan
2 Department of Urology and Andrology, National Hospital of Ministry of Healthcare, Bishkek, Kyrgyzstan
3 Department of Urology and Andrology, I.K.Akhunbaev Kyrgyz State Medical Academy, Bishkek, Kyrgyzstan
4 Faculty of Medicine, Ala-Too International University, Bishkek, Kyrgyzstan
Abstract
Objective: Open prostatectomy remains a standard treatment for large-volume benign prostatic hyperplasia (BPH) in resource-limited settings. Modified retropubic adenomectomy (mRPA) with hemostatic sutures leads to less pronounced bleeding, inflammatory changes and complications in early postoperative period. This study compares the perioperative outcomes of mRPA and transvesical adenomectomy (TVA).
Methods: A retrospective analysis was conducted on 73 patients who underwent open adenomectomy for BPH. Patients were divided into RPA (n=28) and TVA (n=45) groups. The primary endpoint was the perioperative hemoglobin drop. Secondary endpoints included length of hospital stay, improvement in International Prostate Symptom Score (IPSS), and incidence of low-grade complications based on the Clavien-Dindo classification. Comparative analysis was conducted.
Results: Baseline demographics and preoperative IPSS scores were comparable between groups (p˃0.05). mRPA was presented with longer operative time and greater intraoperative blood loss (p<0.001). Despite this, mRPA patients exhibited higher hemoglobin, red blood cell, and hematocrit levels on postoperative 6th day. Additionally, mRPA patients experienced shorter durations of catheterization, irrigation, and hospitalization (p<0.001). Postoperative IPSS scores were significantly better in the mRPA group (p<0.001). The incidence of low-grade Clavien-Dindo complications was similar between groups (p=0.25).
Conclusions: Modified RPA offers advantages in terms of faster hematological recovery, shorter hospital stay, and improved postoperative urinary symptoms compared to TVA in patients with BPH. These findings support the consideration of RPA as a favorable surgical approach for BPH in appropriate clinical settings.
Key words: Benign prostatic hyperplasia, retropubic adenomectomy, bleeding, postoperative hemoglobin drop, length of hospital stay, lower urinary tract symptoms
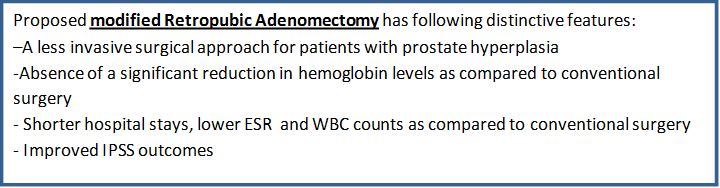
Graphical abstract
Introduction
Benign prostatic hyperplasia (BPH) remains one of the most common urological conditions affecting men older than 60 years, often leading to lower urinary tract symptoms with significantly impaired quality of life (1, 2). While pharmacological and minimally invasive treatments are effective in many cases, a subset of patients with large prostate volumes or complications such as urinary retention, recurrent infections, or bladder stones ultimately require surgical intervention (3, 4).
Open prostatectomy, traditionally performed via a transvesical (suprapubic) approach, has long been the standard treatment for very large prostates, particularly in settings with limited access to advanced minimally invasive technologies such as holmium laser enucleation or robotic surgery. However, the evolution of surgical techniques has brought renewed interest in retropubic adenomectomy (RPA), first popularized by Millin in the mid-20th century (5).
Despite the complexity of procedure and increased intraoperative blood loss, this technique allows direct access to the prostatic adenoma via the retropubic space, without opening the bladder, potentially reducing postoperative bleeding and hospital stay (6, 7).
To date, majority of the robust clinical results were obtained through endoscopic, minimally invasive or robot-assisted surgical options where the role of open surgeries significantly decreased (8). Despite the clearly defined superiority of endoscopic techniques over traditional open surgeries, there is still ongoing debate regarding their clinical advantages over these conventional approaches (9). Comparative studies remain limited; many are small-scale or lack robust clinical endpoints such as perioperative morbidity, hemoglobin drop, postoperative complications, and quality-of-life outcomes.
The present study aims to conduct a comparative analysis of patients who underwent either modified retropubic and transvesical adenomectomy for BPH, with a focus on key clinical outcomes such as perioperative blood loss, length of hospital stay, complication rates, and symptom reduction. By addressing these endpoints, we seek to clarify the potential advantages of the retropubic approach and inform surgical decision-making in settings where open surgery remains a mainstay of treatment.
Methods
Study Design
Single-center retrospective cohort study. The study’s design, participant enrollment, data collection procedures, choice of statistical methods, and interpretation of findings fully adhere to the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) guidelines.
Study population
The study involved 81 adult male patients diagnosed and underwent either modified RPA (mRPA) or transvesical adenomectomy (TVA) in Urology and Andrology Department of National Hospital of the Ministry of Healthcare over four years, from October 2021 to January 2025.Indications for RPA included large prostate volume ˃100ml, failed medical therapy despite the combination of α-blockers and 5α-reductase inhibitors, acute urinary retention (AUR). All modified RPA procedures were performed by a single experienced surgeon, who conducts over 100 such procedures annually, thereby ensuring consistency and proficiency in surgical outcomes.
Inclusion criteria for the study consisted of elective surgery mode, lack of malignancy and availability of complete medical records. Patients were excluded if they had a history of gallstones, bladder diverticulum, adenoma volume <100 cm³, redo prostate operations (e.g., via Key incision), advanced ASA classification, or significant comorbidities that contraindicated surgery and prolonged anticoagulant use prior to surgery, including warfarin and novel oral drugs.
The Ethics Committee of Kyrgyz State Medical Institute of Postgraduate Training and Continuous Education approved and patient confidentiality was maintained throughout the study. Due to the retrospective study design, no informed consent from patients to participate in the study was required; however patients provided consent for all procedures including surgery.
Data collection and variable characteristics
Patient data were extracted from electronic and paper medical records using a standardized data collection form. Demographic characteristics such as age and body mass index (BMI) were reported for adjustment of the study groups. Clinical variables consisted of clinical diagnosis (cystitis, pyelonephritis, nephrolithiasis), comorbidities (diabetes mellitus, arterial hypertension, coronary artery disease and complications of BPH as AUR. Preoperative and postoperative international prostate symptoms scores (IPSS) were evaluated. The IPSS is a validated, patient completed questionnaire comprising seven urinary-symptom questions scored 0–5 (range 0–35), plus one quality of life item scored 0–6. Higher scores indicate more severe lower urinary tract symptoms and worse quality of life (10).
Complete blood cell (CBC) parameters included preoperative and postoperative values, such as red blood cells count (RBC), blood hemoglobin (Hb), hematocrit (Ht), white blood cell count (WBC) and erythrocyte sedimentation rate (ESR) levels. Preoperative urine analysis findings included proteinuria, pyuria and hematuria. Postoperative CBC sampled at 6th day following surgery was included and analyzed in the study. Blood chemistry panel included preoperative glucose, urea, blood urea nitrogen (BUN), fibrinogen, total and free prostate specific antigen (PSA) values. Both of the baseline and post-operative creatinine levels were measured. Baseline ultrasound values included total prostate volume (TPV) and vesical post-void residual volume (PVR).
Surgery
All procedures were performed under epidural anesthesia.
Following midline retropubic access, adenomatous nodules are excised via Millin’s technique in the modified RPA approach, developed and patented by our team (KG Patent N2358) (11). Hemostasis is achieved by placing purse string catgut sutures around the superior and inferior semicircumference of the bladder neck, which include the distal urethral segment and are then tightened to approximate the tissues, preserving bladder integrity without opening the bladder.
Traditional TVA was performed through a suprapubic incision, the bladder is opened, the adenoma was enucleated from within the bladder lumen, and hemostasis was achieved using standard prostatic fossa ligation or suturing. An epicystostomy tube was inserted, and catheterization was carried out per institutional protocol.
Perioperative surgical risk was evaluated following American Society of Anesthesiology (ASA) classification, a surgeon–anesthesiologist consensus score (I–VI, with “E” for emergencies) that evaluates a patient's preoperative comorbidity burden and provides a standardized estimate of perioperative risk (12).
Other variables related to surgery included total operation time, volume of intraoperative blood loss, presence of major bleeding and need for transfusion and insertion of epicystostomy and continuous bladder irrigation system (CBIS). Following the modified RPA surgery, a three-way Foley catheter was used for urinary drainage and CBIS.
In the TVA group, an epicystostomic tube, two-way Foley, or Nelaton catheter was used in combination with CBIS. Notably, catheter and irrigation removal occurred significantly earlier in the mRPA group, contributing to earlier patient mobilization.
Early post-operative complications included presence of incontinency, bladder neck contracture (BNC), urethral stricture, and need for transfusion. Other post-op indicators included duration of catheter days (DCD), need for re-catheterization, early activation day following surgery (EAD), analgesic use, fever and length of hospital stay (LOHS). Postoperative complications were classified using the Clavien-Dindo grading (CDG), which grades complications I (minor deviations) to V (death), based on the required level of therapeutic intervention (13).
Primary and secondary endpoints
The primary endpoint, perioperative hemoglobin drop, was measured by comparing preoperative and postoperative hemoglobin levels obtained at 6th day after surgery. Secondary endpoints included: (1) LOHS, defined as the number of days from surgery to discharge; (2) improvement in IPSS, assessed preoperatively and at a 6-week follow-up; (3) reduction in inflammatory markers, such as ESR and WBC count; and (4) postoperative complications graded according to the CDG, were recorded during the hospital stay.
Statistical analysis
All calculations were achieved by Stata 16.1, Stata Corp, Texas, USA. Continuous variables are denoted by mean and standard deviations when the normal distribution was presented following group-adjusted Shapiro-Wilk test. In case of the violation of normality assumption, median and interquartile ranges are used. Categorical variables are described by absolute count and percentages. For baseline comparison of demographic, clinical and perioperative continuous variables independent samples t-test or Mann-Whitney U test were used according to normality of dataset. For the same purpose of comparison of categorical dataset either Chi-square or Fischer’s exact test were applied. Pre-and postoperative comparison of continuous variables was analyzed by paired samples t-test or Wilcoxon sign test, and changes (delta) of values were compared by t-test/Mann-Whitney U test. Statistical significance was adjusted for two-tailed alfa and p-value of less than 0.05 and 95% of confidence intervals (CI).
Results
General characteristics of population
A total of 81 patients were initially enrolled in the study through convenience sampling. Seven patients were subsequently excluded due to emergency surgical intervention (n=2), diagnosis of malignancy (n=1), and incomplete data (n=5). Consequently, 73 patients met the eligibility criteria and were included in the final analysis. Based on clinical indications and surgeon expertise, 28 patients underwent modified RPA, while 45 patients underwent TVA.
Analysis of demographic and baseline clinical findings
Both of the surgical groups were comparable (Table 1) across all assessed demographic parameters: age, weight, height, and BMI (all p>0.05). Additionally, preoperative IPSS values did not differ significantly between groups (p = 0.67). The prevalence of comorbidities was also similar across both cohorts (p > 0.05).
|
Table 1. Demographic and baseline clinical characteristics of study groups |
||||
|
Variables |
Total |
mRPA (n=28) |
TVA (n=45) |
p |
|
Age, years |
66.8 (5.3) |
67.3(5.4) |
66.5(5.2) |
0.49 |
|
Weight, kg |
81.6(10.5) |
80.7(10.1) |
82.9(10.9) |
0.53 |
|
Height, cm |
176.4(6.3) |
174.5(5.1) |
177.5(6.7) |
0.05 |
|
BMI, m2 |
25.6 (24.3 - 27.7) |
25.8 (24.3 - 27.6) |
25.5 (24.3 - 28.0) |
0.98 |
|
IPSS, points |
29 (28-31) |
29.5 (28.5-31) |
29 (28-31) |
0.67 |
|
AUR, n(%) |
72 (98.6) |
27 (96.4) |
45 (100) |
0.38 |
|
Cystitis, n(%) |
73 (100) |
28 (100) |
45 (100) |
NA |
|
Pyelonephritis, n(%) |
73 (100) |
28 (100) |
45 (100) |
NA |
|
Nephrolithiasis, n(%) |
4 (5.4) |
3 (10.7) |
1 (2.2) |
0.15 |
|
Diabetes mellitus, n(%) |
11 (15) |
5 (17.8) |
6 (13.3) |
0.73 |
|
Arterial hypertension, n(%) |
26 (35.6) |
9 (32.1) |
17 (37.7) |
0.80 |
|
CAD, n(%) |
22 (30.1) |
10 (35.7) |
12 (26.6) |
0.44 |
|
Data are presented as mean (SD), median (interquartile range) or number (%) t-test for independent samples, Mann-Whitney test, Chi-square or Fischer exact test AUR – acute urinary retention, BMI – body mass index, CAD – coronary artery disease, IPSS –International Prostate Symptom Score, mRPA – modified retropubic adenomectomy, NA – non-available, TVA – transvesical adenomectomy |
||||
Analysis of baseline ultrasound and laboratory findings
Comparative analysis revealed no significant differences between the mRPA and TVA groups concerning prostate volume and residual urine volume (both p>0.05). However, the TVA group exhibited significantly higher free PSA levels compared to the mRPA group (p = 0.04). These findings are detailed in Table 2.
|
Table 2. Comparison of baseline laboratory and ultrasound findings of study groups |
||||
|
Variables |
Total |
mRPA (n=28) |
TVA (n=45) |
p |
|
PVR, ml |
598.7(138) |
580.7(151.9) |
610(129.1) |
0.38 |
|
TPV, ml |
140.1(16.1) |
137.5(17.8) |
141.7(15) |
0.28 |
|
RBC, count х 109/L |
4.7 (4.4-5.3) |
5.0 (4.5-5.4) |
4.6 (4.4-5.2) |
0.08 |
|
Hb, mg/dl |
144 (126-153) |
144 (125-156) |
144 (127-149) |
0.53 |
|
Ht, % |
46.5 (45.0-46.5) |
45.5 (43.5-47.5) |
46.5 (46.5-46.5) |
0.07 |
|
ESR, mm/h |
14 (7-18) |
13 (5.5-18) |
15 (8-20) |
0.41 |
|
WBC, count х 106/L |
9.8 (6.1-12) |
8.6 (6.3-11.5) |
10 (6.1-13.6) |
0.20 |
|
TPU, n(%) |
14 (19.1) |
6 (21.4) |
2 (4.4) |
0.76 |
|
Piuria, n(%) |
9 (11.3) |
6 (21.4) |
3 (6.6) |
0.08 |
|
Hematuria, n( %) |
21 (28.7) |
6 (21.4) |
15 (33.3) |
0.30 |
|
Glucose, mmol/l |
5.7 (5.7-5.7) |
5.6 (5.3- 6.0) |
5.7 (5.7-5.7) |
0.54 |
|
Creatinine, mmol/L |
82 (72-90.7) |
77.4 (71.3-89) |
80 (75-91) |
0.05 |
|
Urea, mg/dL |
6.1 (5.5-6.6) |
6.1 (6.1-6.4) |
6.0 (5-7) |
0.05 |
|
BUN, mg/dL |
19 (17-21) |
19 (19-21) |
19 (17-22) |
0.95 |
|
Fibrinogen, mmol/L |
3100 (2900- 3840) |
3526 (2920- 3840) |
2980 (2890- 3552) |
0.42 |
|
PSA total, ng/L |
4 (3.8-4.6) |
4.1 (2.6-4.9) |
4 (3.8-4.3) |
0.61 |
|
PSA free, ng/L |
0.4 (0.3-0.5) |
0.4 (0.3-0.9) |
0.3 (0.3-0.4) |
0.04 |
|
Data are presented as mean (SD), median (interquartile range) or number (%) t-test for independent samples, Mann-Whitney test, Chi-square or Fischer exact test BUN – blood urea nitrogen, ESR –erythrocyte sedimentation rate, Hb –hemoglobin, Ht – hematocrit, mRPA – modified retropubic adenomectomy, PSA – prostate specific antigen, PVR – postvoid residual volume, RBC –red blood cells, TPV – total prostate volume, TPU – trace proteinuria, TVA – transvesical adenomectomy, WBC –white blood cells |
||||
Analysis of postoperative laboratory findings and paired comparisons
In contrast to baseline laboratory values, significant postoperative differences were observed between the mRPA and TVA groups in CBC parameters and ESR (p < 0.05). Patients in the TVA group exhibited lower RBC counts, Hb, and Ht levels, alongside elevated ESR and WBC counts. Recall that, all patients were subjected to standard antibiotic prophylaxis in perioperative period. These findings suggest a more pronounced inflammatory response and potential blood loss in the TVA group. However, postoperative serum creatinine levels did not differ significantly between the groups (p = 0.31), indicating comparable renal function post-surgery. Detailed results are presented in Table 3.
|
Table 3. Postoperative comparative laboratory findings of study groups |
||||
|
Variables |
Total |
mRPA (n=28) |
TVA (n=45) |
p |
|
RBC, count х 109/L |
4.5 (4.1-4.8) |
4.8 (4.3-5.6) |
4.2 (3.9-4.5) |
<0.001 |
|
Hb, mg/dl |
128.6(18.0) |
140.1(11.2) |
121.4(17.7) |
<0.001 |
|
Ht, % |
35.1 (32.1-37.8) |
37.1 (34.2-39.6) |
33.7 (32.1-36.2) |
0.007 |
|
ESR, mm/h |
16 (11-22) |
13 (7-16.5) |
19 (14-26) |
0.009 |
|
WBC, count х 106/L |
8.6 (6-11) |
6.8 (3.6-9.2) |
10 (6.9-15) |
<0.001 |
|
Creatinine, mmol/L |
83 (79-85.5) |
82 (79.6-84.9) |
85 (78-87) |
0.31 |
|
Data are presented as mean (SD) and median (interquartile range) t-test for independent samples, Mann-Whitney test ESR-erythrocyte sedimentation rate, Hb –hemoglobin, Ht –hematocrit, mRPA –modified retropubic adenomectomy, RBC – postoperative red blood cells, TVA – transvesical adenomectomy, WBC –white blood cells |
||||
Paired analyses within the TVA group (Table 4) demonstrated statistically significant postoperative changes across all CBC parameters and serum creatinine levels (p < 0.05). In contrast, the mRPA group did not exhibit significant alterations in these parameters (p > 0.05).
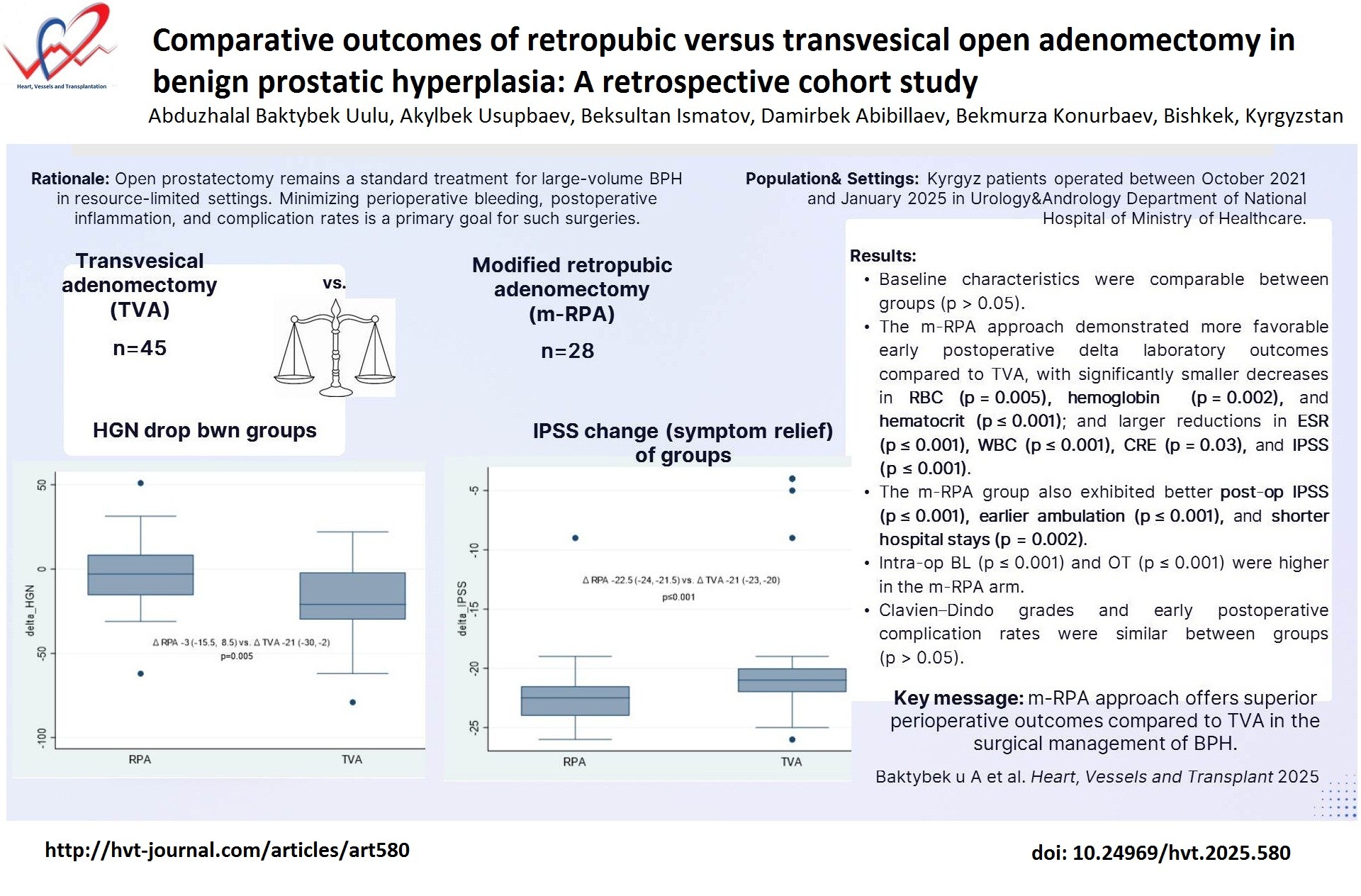
Furthermore, intergroup comparisons of these changes revealed significant differences between the TVA and mRPA groups for all analyzed variables (p < 0.05), indicating a more pronounced postoperative hematological and renal impact associated with the TVA procedure. These findings arepresented in Table 4 and highlighted in Figures 1- 3.
|
Table 4. Comparison of laboratory findings and IPSS in study groups before and after surgery |
|||||
|
Variables |
mRPA before –after surgery p* |
Δ mRPA** |
TVA before after surgery p* |
ΔTVA** |
Δ p |
|
RBC count х 109/L |
0.44 |
-0.06 (0.6) |
0.44 |
-0.57(0.82) |
0.005 |
|
Hb, mg/dL |
0.28 |
-3 (-15.5, 8.5) |
0.28 |
-21 (-30, -2) |
0.002 |
|
Ht,% |
0.07 |
-8.2(2.2) |
0.07 |
-11.5(3.5) |
<0.001 |
|
ESR, mm/h |
0.41 |
0.6 (-3.3, 2.1) |
0.41 |
2 (1, 7) |
<0.001 |
|
WBC count х 106/L |
0.001 |
-1.9 (-3.3, -1) |
0.001 |
1 (-1, 2) |
<0.001 |
|
Creatinine, mmol/L |
0.24 |
3.5 (-6.5, 13.8) |
0.24 |
-2 (-4, 5) |
0.03 |
|
IPSS, points |
<0.001 |
-22.5 (-24, -21.5) |
<0.001 |
-21 (-23, -20) |
<0.001 |
|
Data are presented as mean (SD) and median (interquartile range) *t-test for dependent samples, Wilcoxon test **t-test for independent samples, Mann-Whitney test ESR – erythrocyte sedimentation rate, Hb –hemoglobin, Ht –hematocrit, IPSS - International Prostate Symptom Score, mRPA –modified retropubic adenomectomy, RBC – red blood cells, TVA – transvesical adenomectomy, WBC – postoperative white blood cells |
|||||
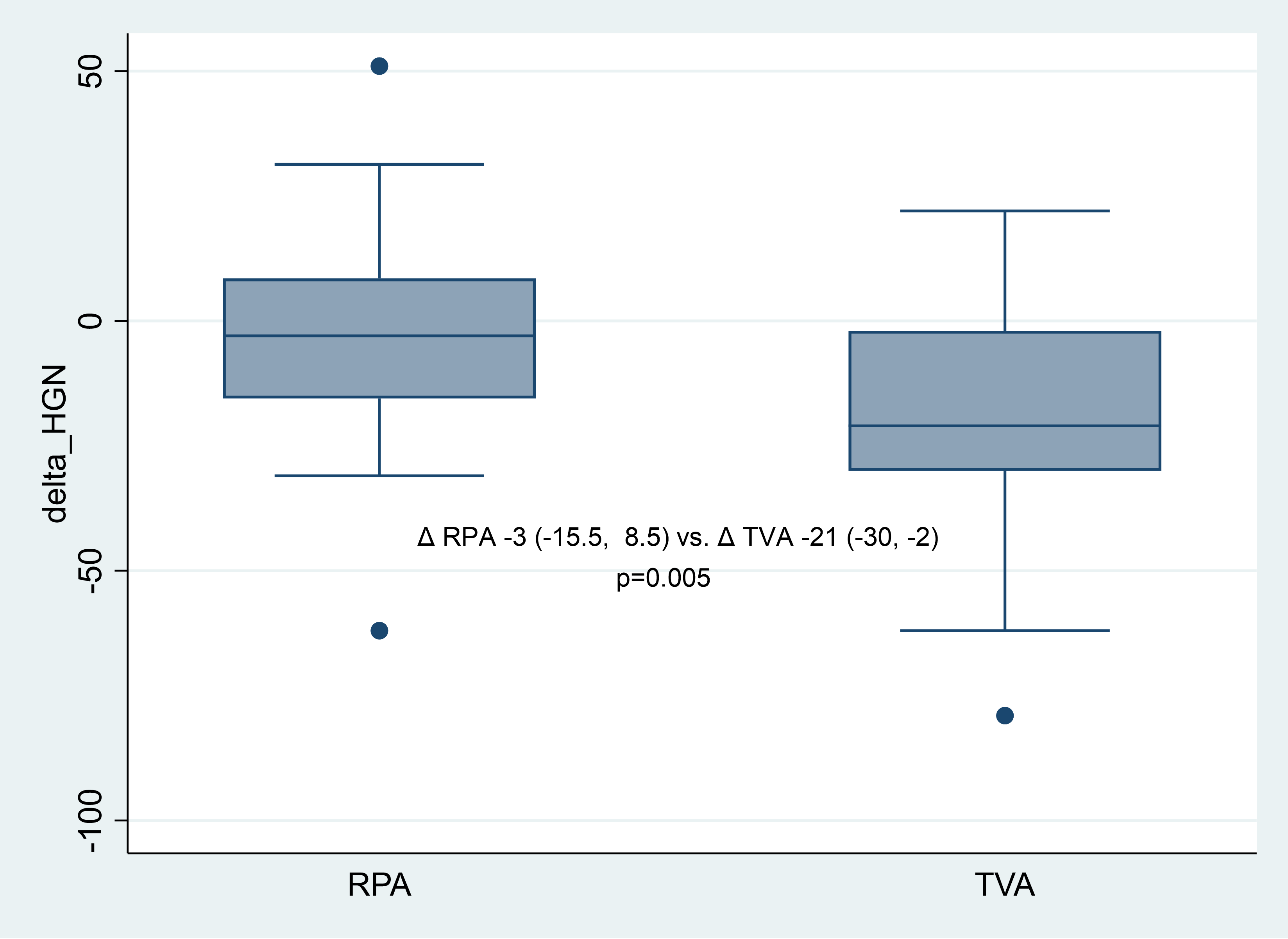
Figure 1. Comparison of postoperative hemoglobin drops between surgery groups
HGN- hemoglobin, RPA –modified retropubic adenomectomy, TVA – transvesical adenomectomy![]()
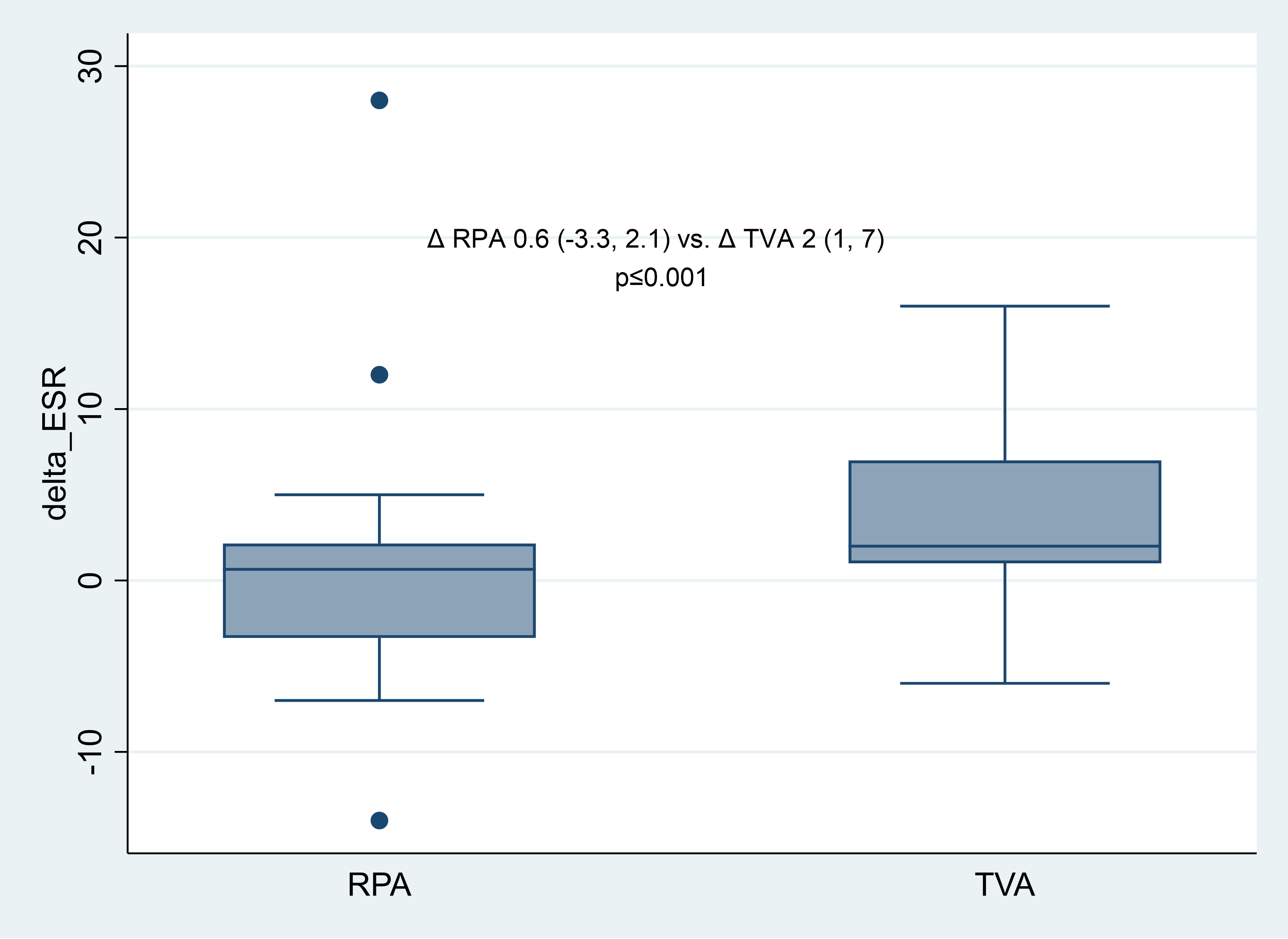
Figure 2. Comparison of postoperative ESR shifts between surgery groups
ESR – erythrocyte sedimentation rate, RPA –modified retropubic adenomectomy, TVA – transvesical adenomectomy
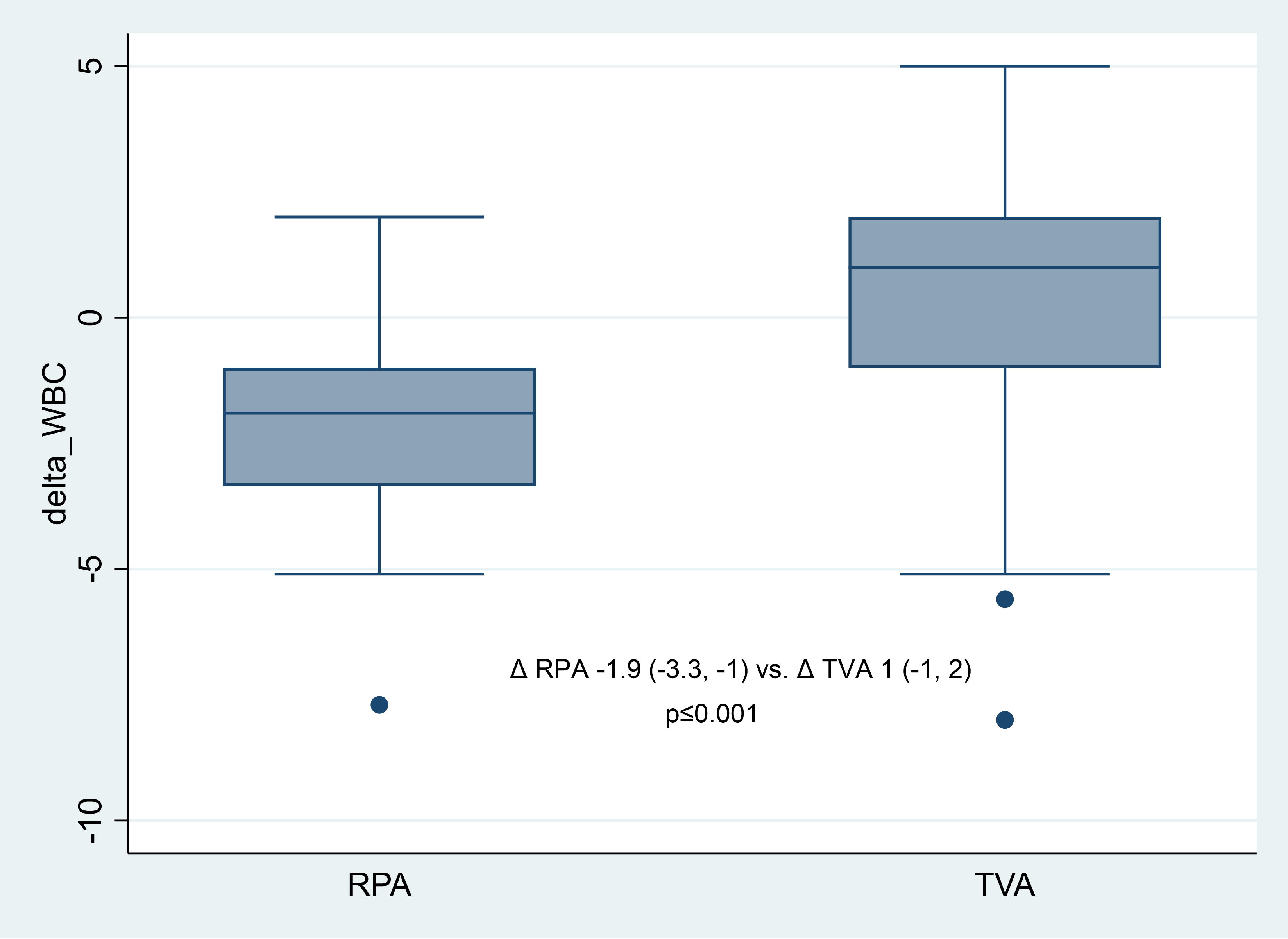
Figure 3. Comparison of postoperative WBC changes between surgery groups
WBC – white blood count, RPA –modified retropubic adenomectomy, TVA – transvesical adenomectomy
Analysis of perioperative clinical and surgical findings
The two surgical groups (Table 5) were comparable regarding the ASA physical status classification (p = 0.32). The operative time was significantly longer in the mRPA group (p < 0.001), and intraoperative blood loss was also higher in this cohort (p < 0.001). However, no cases required blood transfusion associated with significant bleeding. Epicystostomy was implemented in all TVA patients, whereas it was necessary in only one case within the mRPA group (p < 0.001).
To prevent the bladder tamponade, CBIS was employed for all patients. The duration of irrigation differed significantly between groups, being notably shorter in the mRPA group (p < 0.001). Similarly, the duration of catheterization was significantly reduced in the mRPA group (p < 0.001). These factors contributed to earlier mobilization in the mRPA group (p < 0.001), resulting in a significantly shorter hospital days (p < 0.001).
Postoperative lower urinary tract symptoms, assessed via the IPSS, were significantly more pronounced in the TVA group compared to the mRPA group (p < 0.001). Paired comparisons are presented in Table 4., where IPSS was significantly decreased in both groups (p < 0.001).
According to the CDG of surgical complications, most patients experienced Grade I complications, with some instances of Grades II and III. The distribution of complication grades was comparable between groups (p = 0.25). Isolated cases of BNC and urinary incontinence were observed without significant intergroup differences (p > 0.05). Analgesic use in the early postoperative period was common across both groups due to incision site pain (p = 0.62). A few patients developed postoperative fever, with no significant difference between groups (p = 0.28). Comprehensive results are detailed in Table 5.
|
Table 5. Comparison of perioperative clinical and surgical findings in study groups |
||||
|
Variables |
Total |
mRPA (n=28) |
TVA (n=45) |
p |
|
ASA class, n(%) II III |
39 (53.4) 34 (46.6) |
17 (60.7) 11 (39.3) |
22 (48.9) 23 (51.1) |
0.32 |
|
OT, min |
87 (80-90) |
90 (88-94.5) |
82 (74-88) |
<0.001 |
|
Intraoperative blood loss, ml |
113.5(24.8 |
138.6(16.5) |
97.9(13.8) |
<0.001 |
|
LOHS, days |
11 (10-11) |
10 (8-11) |
11 (10-11) |
0.002 |
|
Epicystostomy, n(%) |
46 (63.1) |
1 (3.6) |
45 (100) |
<0.001 |
|
CBIC, days |
5 (1-5) |
1 (1-1) |
5 (5-6) |
<0.001 |
|
Catheter insertion, days |
10 (9-10) |
9 (9-10) |
10 (10-11) |
<0.001 |
|
EAD, days |
5 (2-6) |
2 (2-2) |
6 (5-6) |
<0.001 |
|
Repeated catheter insertion, n(%) |
5 (6.8) |
1 (3.6) |
4 (8.9) |
0.64 |
|
BNC, n(%) |
5 (6.8) |
1 (3.6) |
4 (8.9) |
0.64 |
|
Urinary incontinence, n(%) |
2 (2.7) |
0 |
2 (4.4) |
0.52 |
|
Post-IPSS, points |
8 (7-9) |
7 (6-7) |
8 (7-9) |
<0.001 |
|
Analgesic use, n(%) |
71 (97.2) |
27 (96.4) |
44 (97.8) |
0.62 |
|
Fever, n(%) |
3 (4.1) |
0 |
3 (6.7) |
0.28 |
|
CDG, n(%) Grade 1 Grade 2 Grade 3 |
64 (87.6) 4 (5.5) 5 (6.8) |
27 (96.4) 0 1 (3.7) |
37 (82.2) 4 (8.9) 4 (8.9) |
0.25 |
|
Data are presented as median (interquartile range) or number (%) Mann-Whitney test, Chi-square or Fischer exact test ASA – American society of anesthesiology, BNC – bladder neck contracture, CBIS – continuous bladder irrigation system, CDG – Clavien-Dindo grading, EAD – early activation day, LOHS – length of hospital stay, OT – operation time, mRPA –modified retropubic adenomectomy, post-IPSS – postoperative International Prostate Symptom Score, TVA – transvesical adenomectomy |
||||
![]()
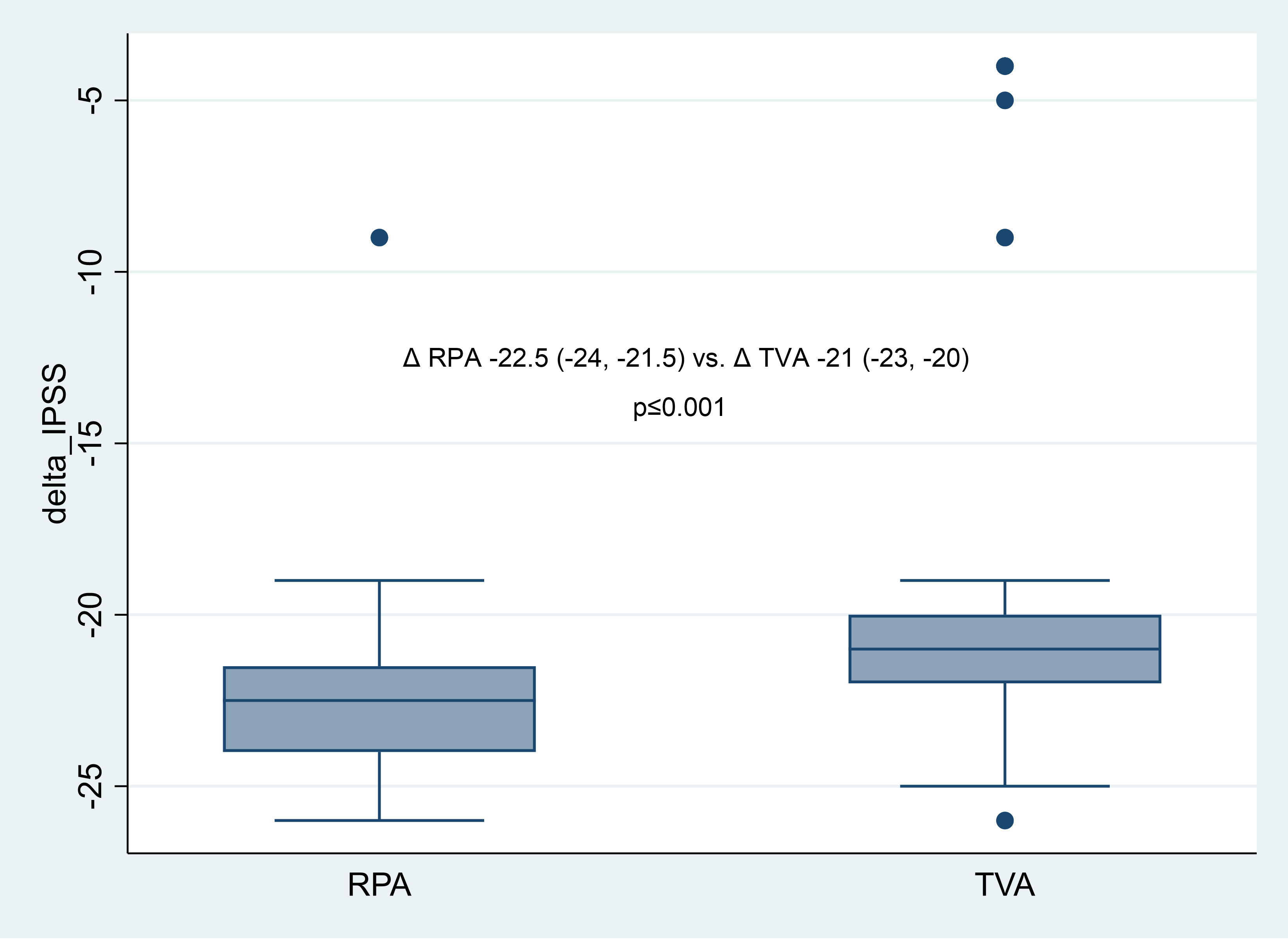
Figure 4. IPSS change comparison by study groups
International Prostate Symptom Score, RPA –modified retropubic adenomectomy, TVA – transvesical adenomectomy
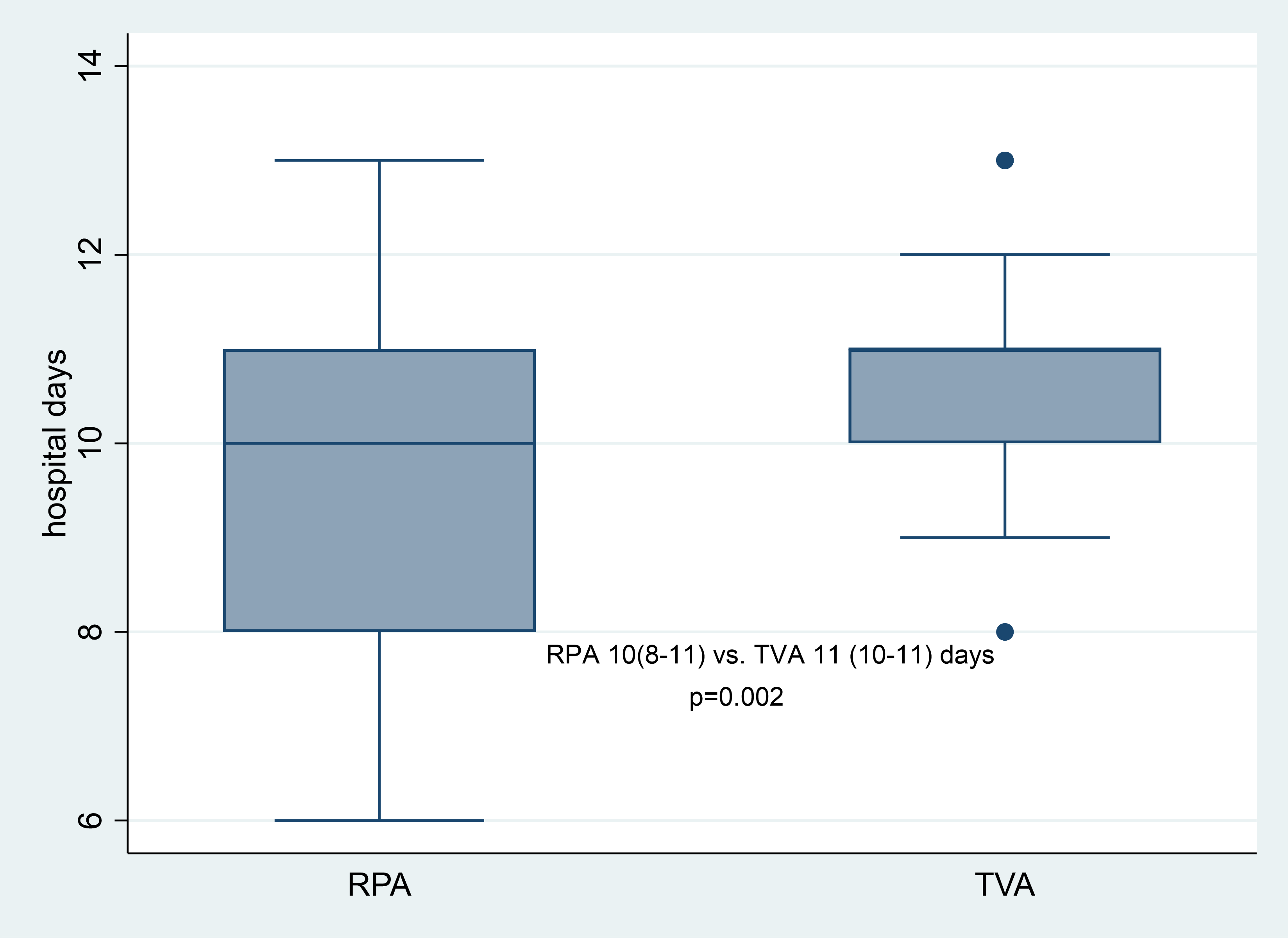
Figure 5. Postoperative LOHS comparison by study groups
LOHS – length of hospital stay, RPA –modified retropubic adenomectomy, TVA – transvesical adenomectomy
Discussion
The absence of a significant reduction in hemoglobin levels in the mRPA group suggests that this technique offers a less invasive surgical approach, thereby achieving our primary endpoint. Furthermore, the mRPA group demonstrated shorter hospital stays, lower ESR WBC counts, and improved IPSS outcomes, highlighting the potential benefits of mRPA as reflected in our secondary endpoints. These findings are consistent with outcomes reported for laparoscopic analogues of RPA (6, 14). Notably, in contrast to the findings reported by Volkov et al. (14), our study did not observe any instances of urinary tamponade among patients undergoing the mRPA procedure.
The comparable baseline characteristics between the two groups, including age, BMI, and comorbidities, suggest that the observed differences in outcomes are attributable to the surgical approach rather than patient-related factors. Specifically, the mRPA group maintained stable postoperative CBC parameters and creatinine levels, whereas the transvesical group exhibited significant declines in red blood cell count, hemoglobin, hematocrit, and elevations in WBC count and ESR. These hematological changes in the TVA group may reflect a more pronounced inflammatory response, greater intraoperative blood loss, and higher Clavien-Dindo complication grades (15, 16).
Interestingly, while the mRPA group experienced longer operative times and greater intraoperative blood loss, they exhibited relatively higher hemoglobin, RBC, and hematocrit levels in the postoperative period compared to the TVA group. This suggests a more favorable hematological recovery trajectory in mRPA patients. Several factors might contribute to this phenomenon. The modified retropubic technique with hemostatic sutures, despite its invasiveness, may allow for more effective hemostasis during surgery, leading to reduced postoperative bleeding. Additionally, the less extensive tissue manipulation in mRPA could result in a lesser extent of inflammatory response. This observation aligns with findings from previous studies, where surgical techniques with efficient intraoperative hemostasis correlated with better postoperative hematological parameters (17, 18). For instance, a study comparing monopolar and bipolar transurethral resection of the prostate found that deeper coagulation depth in bipolar resection led to less bleeding and better postoperative hemoglobin levels (18).
The universal application of continuous bladder irrigation in both groups aimed to mitigate bladder tamponade. However, the mRPA group benefited from significantly shorter irrigation durations, aligning with the reduced intraoperative blood loss observed. Furthermore, epicystotomy was not necessitated in the mRPA group, indicating a less invasive postoperative course. These factors likely influenced patients' quality of life by facilitating early mobilization and resulting in lower postoperative IPSS values in the mRPA group. This finding suggests that mRPA may offer better preservation of urinary function and patient comfort in the immediate postoperative period. The impact of early mobilization is supported by large-scale studies on enhanced recovery after urologic surgery (19).
Study limitations
This study's limitations include its retrospective design and the relatively small sample size. Additionally, the study did not assess long-term functional outcomes, such as urinary continence and sexual function, which are important considerations in BPH surgery. Due to the large prostate volumes (>100 cm³) and the chronic nature of lower urinary tract symptoms in our patient population, most patients had been prescribed empirical antibiotics prior to admission. As a result, urine cultures often lacked clinical utility and were not routinely collected at the time of admission. Future prospective, randomized studies with larger cohorts and extended follow-up periods are warranted to confirm these results and to evaluate the long-term functional outcomes associated with each surgical approach.
Conclusions
The findings suggest that our technique may offer superior perioperative outcomes compared to TVA in the surgical management of BPH. While the overall complication rates, classified according to the Clavien-Dindo grading, were similar between groups, the modified RPA group experienced fewer severe complications. The absence of significant differences in analgesic requirements and postoperative fever indicates comparable pain management and infection control in both surgical approaches.
Ethics: The Ethics Committee of Kyrgyz State Medical Institute of Postgraduate Training and Continuous Education approved and patient confidentiality was maintained throughout the study. Due to the retrospective study design, no informed consent from patients to participate in the study was required; however, patients provided consent for all procedures including surgery.
Peer-review: External and internal
Conflict-of-interest: None to declare
Author contributions: A.B., A.U. and B.I. – data collection, database entry and preprocessing, manuscript conceptualization; D.A. and B.K. – methodology, statistical analysis and manuscript writing. All authors critically reviewed final version, thus fulfilled all authorship criteria
Acknowledgement and Funding: None to declare
Statement on A.I.-assisted technologies use: Authors declare that, Open AI product Chat GPT 4.0 was used in the generation of ideas on study design and manuscript preparation but authors take responsibility for whole manuscript writing process
Availability of data and material: Contact authors. In case sharing of data is granted fair use rules apply with acknowledgement of source and /or collaboration
References
| 1.Infante Hernández S, Gómez Rivas J, Moreno Sierra J. Benign prostatic hyperplasia. Hiperplasia benigna de próstata. Med Clin (Barc) 2024; 163: 407-14. doi:10.1016/j.medcli.2024.04.014 https://doi.org/10.1016/j.medcli.2024.04.014 PMid:39013719 |
||||
| 2.Ng M, Leslie SW, Baradhi KM. Benign prostatic hyperplasia. (Updated 2024 Oct 20). In: StatPearls (Internet). Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: URL: https://www.ncbi.nlm.nih.gov/books/NBK558920/ | ||||
| 3.Helman TA, Browne BM. Advances in outpatient therapies and treatment of benign prostatic hyperplasia: A comprehensive review for men's health. Med Clin North Am 2024; 108: 981-91. https://doi.org/10.1016/j.mcna.2024.03.009 PMid:39084845 |
||||
| 4.de la Rosette JJ, Alivizatos G, Madersbacher S, Perachino M, Thomas D, Desgrandchamps F, et al. European Association of Urology. EAU Guidelines on benign prostatic hyperplasia (BPH). Eur Urol 2001; 40: 256-63. https://doi.org/10.1159/000049784 PMid:11684840 |
||||
| 5.Fitzpatrick JM. Millin retropubic prostatectomy. BJU Int 2008; 102: 1486. doi:10.1111/j.1464-410X.2008.07925.x https://doi.org/10.1111/j.1464-410X.2008.07925.x PMid:18821926 |
||||
| 6.Eremenko SN, Eremenko AN, Mykhaylichenko VYu, Dolgopolov VP, Chernega VS, Khalilova AS-A. Laparoscopic retropubic extraurethral adenomectomy. Vestn Urol 2022; 10: 43-52. doi:10.21886/2308-6424-2022-10-2-43-52 https://doi.org/10.21886/2308-6424-2022-10-2-43-52 |
||||
| 7.Shkodkin SV, Idashkin YuB, Zolotukhin DA, Fironov SA, Nevskiy AA. The role of retropubic adenomectomy at the present stage. Vestn Bashkirskogo Gos Med Univ 2019; 5: 390-1. | ||||
| 8.Noguera RS, Rodríguez RC. Open adenomectomy: past, present and future. Curr Opin Urol 2008; 18: 34-40. doi:10.1097/MOU.0b013e3282f0d625 https://doi.org/10.1097/MOU.0b013e3282f0d625 PMid:18090487 |
||||
| 9.Sfredo LR, Oliveira IC, Novakoski GKO, Digner IDS, Da Silva IVM, Lacerda DAM, et al. Comparative analysis between open transvesical and laparoscopic adenomectomy in the treatment of benign prostatic hyperplasia in a tertiary hospital in Curitiba-PR: a retrospective study. Rev Col Bras Cir 2023; 50: e20233450. doi:10.1590/0100-6991e-20233450-en https://doi.org/10.1590/0100-6991e-20233450-en PMid:37075466 PMCid:PMC10508660 |
||||
| 10.Barry MJ, Fowler FJ Jr, O'leary MP, Bruskewitz RC, Holtgrewe HL, Mebust WK, et al. The American Urological Association symptom index for benign prostatic hyperplasia. J Urol 2017; 197: S189-97. doi:10.1016/j.juro.2016.10.071 https://doi.org/10.1016/j.juro.2016.10.071 PMid:28012747 |
||||
| 11.Usupbaev AC, Baktybek uulu A, Adiev AT, Akylbek S, Turgunbaev TE inventor; National Hospital of Ministry of Healthcare, assignee. Retropubic adenomectomy with hemostatic sutures. KG Patent No. 2358. December 22, 2022. | ||||
| 12.Mayhew D, Mendonca V, Murthy BVS. A review of ASA physical status - historical perspectives and modern developments. Anaesthesia 2019; 74: 373-9. doi:10.1111/anae.14569 https://doi.org/10.1111/anae.14569 PMid:30648259 |
||||
| 13.Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 2009; 250: 187-96. doi:10.1097/SLA.0b013e3181b13ca2 https://doi.org/10.1097/SLA.0b013e3181b13ca2 PMid:19638912 |
||||
| 14.Volkov SN, Tereshchenko VI, Stepanchenko VS, Mikheev RK, Grigoryan OR, Andreeva EN, et al. Arterial-mediated modifications of surgical treatment for benign prostatic hyperplasia. Exp Clin Urol 2023; 16: 60-8. doi: 10.29188/2222-8543-2023-16-3-60-68 https://doi.org/10.29188/2222-8543-2023-16-3-60-68 |
||||
| 15. Adashchik VG, Strotskiy AV. Transvesical adenomectomy complications after use of various techniques for gland bed hemostasis. Healthcare 2020; 8: 5-11. | ||||
| 16.Sharma V, Meeks JJ. Open conversion during minimally invasive radical prostatectomy: impact on perioperative complications and predictors from national data. J Urol 2014; 192: 1657-62. doi:10.1016/j.juro.2014.06.029 https://doi.org/10.1016/j.juro.2014.06.029 PMid:24936721 |
||||
| 17.Utlu A, Aksakalli T, Celik F, Cinislioglu AE, Demirdogen SO. The effect of hemostatic sutures on open suprapubic prostatectomy outcomes: A retrospective observational study. Actas Urol Esp 2025; 49: 501711. doi:10.1016/j.acuroe.2025.501711 https://doi.org/10.1016/j.acuroe.2025.501711 PMid:39952560 |
||||
| 18.Huang X, Wang L, Wang XH, Shi HB, Zhang XJ, Yu ZY. Bipolar transurethral resection of the prostate causes deeper coagulation depth and less bleeding than monopolar transurethral prostatectomy. Urology 2012; 80: 1116-20. doi:10.1016/j.urology.2012.07.024 https://doi.org/10.1016/j.urology.2012.07.024 PMid:22990062 |
||||
| 19.Pessoa RR, Urkmez A, Kukreja N, Kukreja JB. Enhanced recovery after surgery review and urology applications in 2020. BJUI Compass 2020; 1: 49-55. doi:10.1002/bco2.9 https://doi.org/10.1002/bco2.9 PMid:35474909 PMCid:PMC8988792 |
||||
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

