Experience of surgical correction of congenital high intestinal obstruction in newborns
ORIGINAL RESEARCH ARTICLE
Experience of surgical correction of congenital high intestinal obstruction in newborns
Article Summary
- DOI: 10.24969/hvt.2025.585
- CARDIOVASCULAR DISEASES
- Published: 22/08/2025
- Received: 20/04/2025
- Revised: 08/08/2025
- Accepted: 08/08/2025
- Views: 1625
- Downloads: 1238
- Keywords: Congenital high intestinal obstruction, duodenal atresia, jejunal atresia, annular pancreas, embrionic adhesions, laparotomy
Address for Correspondence: Tatyana .A. Akmentieva, National Center for Maternal and Child Health, Bishkek, Kyrgyzstan
E-mail: akmen-ta@yandex.ru ORCID: Tatyana A. Akmentieva – 0009-0000-4043-9278
Tatyana A. Akmentieva, Kamchibek A. Uzakbaev, Natalia .F. Gagloeva
National Center for Maternal and Child Health, Bishkek, Kyrgyzstan
Abstract
Objective: The article presents data, selection criteria, and results of surgical treatment of children with congenital high intestinal obstruction (CHIO) who were hospitalized with this pathology in the neonatal intensive care unit (ICU) for surgical pathology at the National Center for Maternal and Child Health in Bishkek, Kyrgyzstan.
The purpose of the study was to develop approaches of diagnosis, surgical treatment, and postoperative management of newborns with CHIO and reduction of postoperative complications.
Methods: From 2016 to 2024, 58 newborns with CHIO were admitted to the ICU for newborns with surgical pathology as duodenal obstruction, which included complete duodenal membrane, duodenal atresia, compression of the duodenum by the ring-shaped head of the pancreas, atresia of the initial section of the jejunum, and embryonic adhesions that compressed the duodenum.
Results: Multiple birth defects were detected in newborns with CHIO, with combined congenital heart defects and Down syndrome noted in 22 (38%) patients. All children underwent preoperative preparation, which included correction of metabolic, hemodynamic disorders, normalization of body temperature and adequate diuresis. The algorithm of diagnostic examinations included clinical-laboratory and radiologic methods, such as X-ray passage of the gastrointestinal tract and irrigography of the large intestine, ultrasonography and ultrasound examination of internal organs. On radiological examination, the presence of ``double bubble`` sign, characterized by two air bubbles in the stomach and dilated part of the duodenum. All newborns underwent surgery: bypass gastrojejunostomy with Brown's anastomosis, duodenotomy, end-to-end small intestine anastomosis and separation of congenital embryonic adhesions. The mortality rate at 3 months after surgery was 3.4%.
Conclusion: The study allowed for a thorough approach to the issues of surgical correction of CHIO in newborns. Analysis of clinical data showed that individual selection of surgical intervention tactics, taking into account the anatomical and physiological characteristics of the patient, timely diagnosis, and subjective postoperative management contribute to a reduction in the frequency of complications and mortality in the early postoperative period. Thus, timely diagnosis of fetal malformations during the antenatal period allows for the determination of treatment tactics and improvement of postoperative outcomes. CHIO in newborns requires various types of surgical intervention on the gastrointestinal tract, and a well-established algorithm for surgical correction of a specific type of congenital intestinal obstruction will improve the treatment outcomes for newborns with this pathology.
Key words: Congenital high intestinal obstruction, duodenal atresia, jejunal atresia, annular pancreas, embrionic adhesions, laparotomy.
Graphical abstract
Introduction
According to WHO data, up to 5–6% of children are born with developmental defects each year, of whom more than 300,000 die within the first 4 weeks of life. Gastrointestinal tract (GIT) abnormalities are the second most common type of defect, surpassed only by heart defects. The most common cause of congenital intestinal obstruction is atresia. Atresia is more often localized in areas of “complex” organogenesis: the esophagus, duodenum, distal ileum, and the junction of the small intestine and large intestine (1).
The most common pathology in neonatal surgery is congenital intestinal obstruction, which is recorded at a frequency of 1:2000 newborns (2). This is explained not so much by an absolute increase in their number as by improvements in diagnosis, both in utero and in the neonatal period. The vast majority of cases of various forms of congenital high bowel obstruction occur during the neonatal period and up to 3 months of age (3, 4). However, issues related to diagnosis, adequate surgical treatment, and postoperative management of this category of patients remain controversial.
Congenital high intestinal obstruction (CHIO) is a form of intestinal obstruction in newborns in which the obstruction to the passage of intestinal contents is located in the proximal (upper) sections of the GIT, most often at the level of the duodenum, jejunum, or initial section of the ileum. This condition requires urgent surgical intervention, as it can lead to severe metabolic disorders, aspiration, intestinal perforation, and death if treatment is delayed.
The most common causes of CHIO include:
• Atresia or stenosis of the duodenum and jejunum,
• Annular pancreas,
• Malrotation of the intestine with volvulus,
• Meckel's diverticulum with intussusception (less common in the neonatal period),
• Meconium plug in the upper sections in cystic fibrosis (rare) (5, 6).
Duodenal atresia is a congenital form of high intestinal obstruction in which there is a complete or partial absence of the lumen of the duodenum.
The incidence is 1 case per 5,000-10,000 newborns, making this pathology highly relevant (7). Often, intestinal malformation can be associated with other congenital developmental abnormalities, including Down syndrome, congenital heart defects, annular pancreas, and malrotation. Pathogenetically, abnormalities in the development of the duodenum and the remaining sections of the small intestine are different, so we consider it appropriate to consider these groups of patients separately.
The diversity of pathomorphological variants of intestinal tube defects complicates the choice of not only the surgical treatment strategy for a particular type of congenital pathology, but also the technique of interintestinal anastomosis itself (6).
The aim of the stud was to develop approaches to the diagnosis, surgical treatment, and postoperative management of newborns with congenital high intestinal obstruction and to reduce the level of postoperative complications.
Methods
Study design and population
In this retrospective descriptive study, 58 newborns who underwent surgery for CHIO between 2016 and 2024, and were treated in the neonatal intensive care unit (ICU) for surgical pathology at the National Center for maternal and child health in Bishkek, Kyrgyzstan were included. This group consisted of children with duodenal obstruction: complete duodenal membrane, duodenal atresia, compression of the duodenum by the ring-shaped head of the pancreas, atresia of the initial section of the jejunum, and embryonic adhesions that compressed the duodenum.
The informed consent parents or guardians of newborns for all procedures, including surgery was obtained. The approval of Institutional Ethical Committee was not required for retrospective study.
Data collection
We collected demographic as age and sex, prematurity index, type of duodenal obstruction, associated congential defects, laboratory, radiological (gastrointestinal tract X-ray and colon irrigation) and ultrasonography data. We recorded the details of preoperative management and preparation of newborns to surgery, intraoperative and postoperative management, type of surgery, complications and morality.
Statistical analysis
Data are presented as number and percentage.
Results and discussion
Of 58 cases of CHIO, boys predominated, with 36 newborns (62%) compared to 22 girls (38%) (Fig. 1).
Premature babies at 34-35 weeks of gestation, accounted for 28 newborns (48%) (Fig. 2).
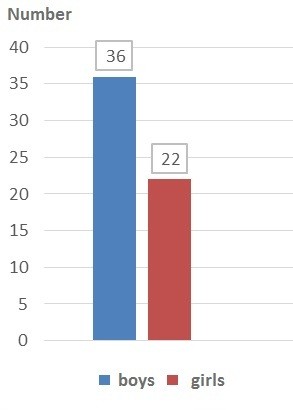
Figure 1. Distribution of patients with congenital high intestinal obstruction by sex
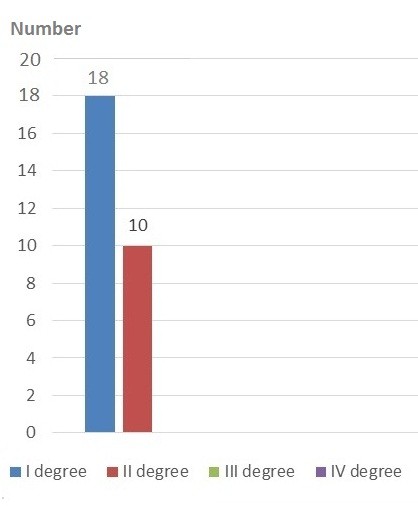
Figure 2. Distribution of newborns with congenital high intestinal obstruction by degree of prematurity
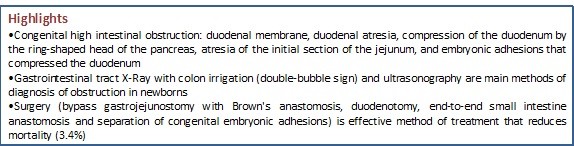
The causes of obstruction were: complete duodenal membrane in 9 (15.5%) patients, duodenal atresia in 15 (26%) children, compression of the duodenum by the ring-shaped head of the pancreas in 25 (43%) newborns, atresia of the initial section of the jejunum in 3 (5.2%) children, and in 5 (9%) children there were embryonic adhesions that compressed the duodenum (Fig. 3).
Of the 58 newborns, the most common causes of CHIO were anomalies associated with compression of the duodenum by the annular pancreas, which accounted for 43% of cases.
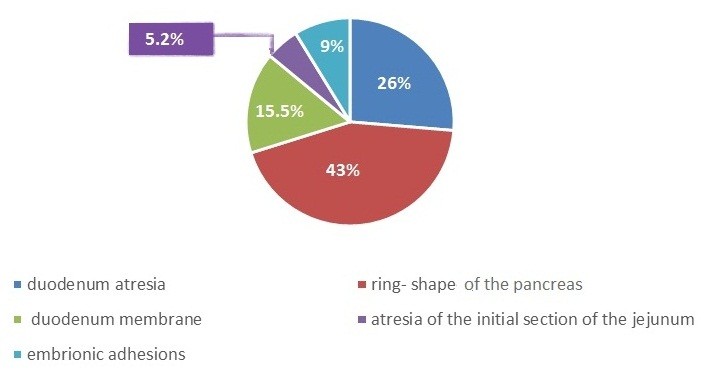
Figure 3. Distribution of patients by the type of congenital high intestinal obstruction
Most often, multiple birth defects were detected in newborns with CHIO, with combined congenital heart defects and Down syndrome noted in 22 (38%) patients.
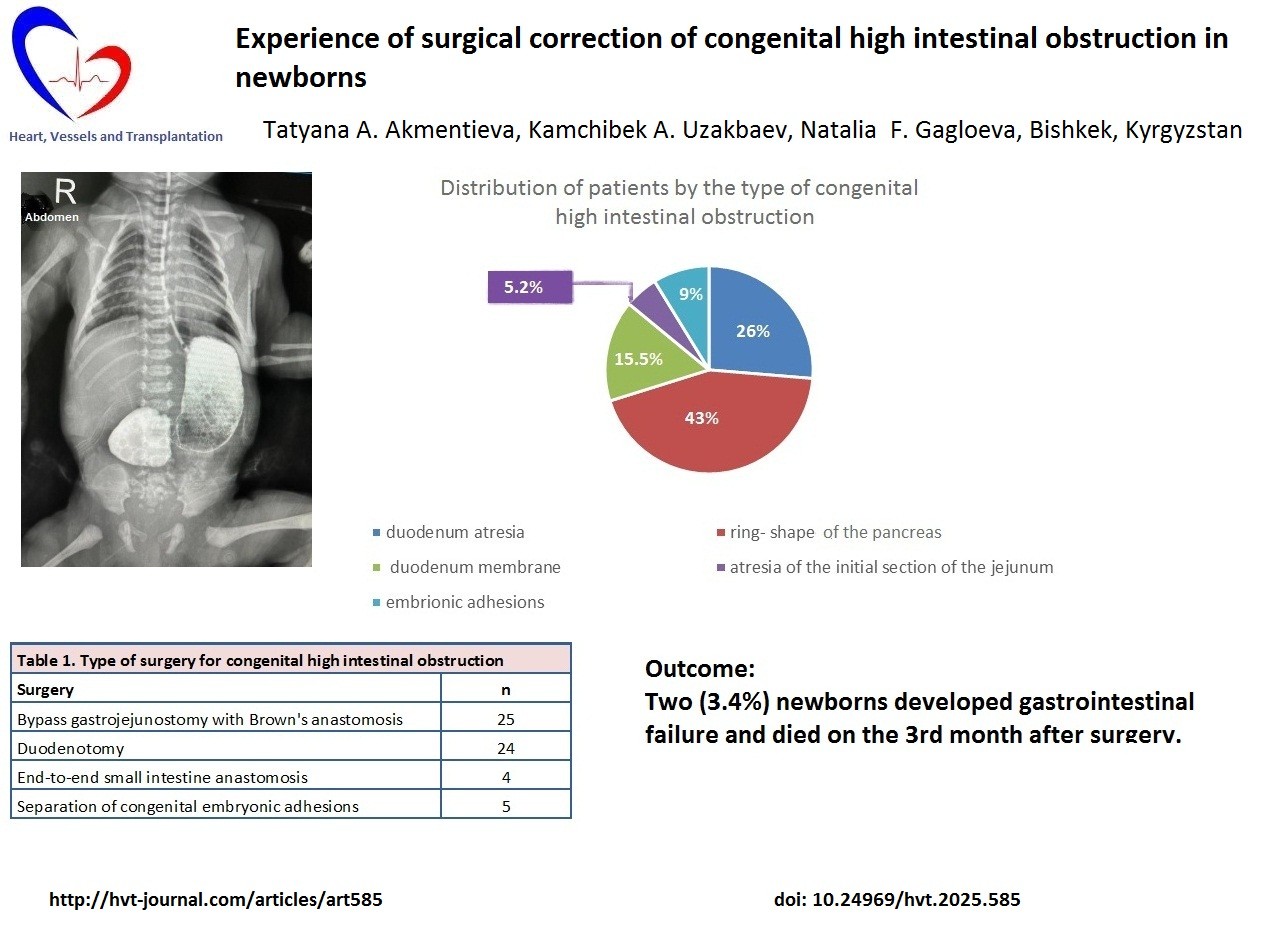
After preoperative preparation, all newborns underwent surgery. Preoperative preparation included correction of metabolic and hemodynamic disorders, normalization of body temperature, and adequate diuresis. The diagnostic examination algorithm included clinical laboratory and radiological methods, as well as special radiological examination methods, such as gastrointestinal tract X-ray and colon irrigation, ultrasonography, and ultrasound examination of internal organs. In radiological examination, the presence of the ``double bubble`` sign is characteristic, characterized by two air bubbles in the stomach and the dilated part of the duodenum. Another method for diagnosing this defect is FEGDS, but in newborns, there is a high risk of perforation of the gastrointestinal tract above the membrane area. Therefore, we consider it appropriate to use a comprehensive approach in the preoperative diagnosis of high congenital intestinal obstruction combining ultrasound diagnostics and X-ray methods as complementary examinations (Fig. 4).
Surgical intervention was performed after preoperative preparation, the duration and nature of which were determined depending on the type of defect, the time of admission, the presence of complications, the severity of the child's condition, and body weight deficiency. For operations related to CHIO, upper median laparotomy was used. This approach allowed free manipulation of the upper GIT. Since the most common structure of high congenital obstruction was a ring-shaped pancreas, the preferred method of surgical treatment was gastrojejunostomy with a Brown's anastomosis, and if it was impossible to perform a duodenal anastomosis (10). In cases of duodenal atresia, a side-to-side anastomosis between the proximal and distal segments of the duodenum was performed using an open technique or duodenojejunostomy (8). Furthermore, if atresia of the initial section of the jejunum was detected during surgery, end-to-end anastomosis was performed (9, 11).
The surgical correction options for anomalies causing high intestinal obstruction are presented in Table 1.
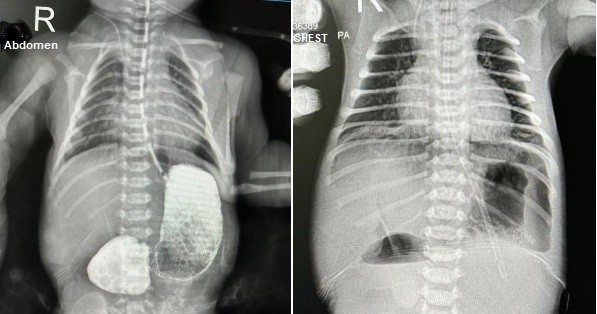
Figure 4. ``Doube-bubble`` sign of intestine on X-Ray
|
Table 1. Surgical correction methods for anomalies causing high intestinal obstruction in newborns |
|
|
Surgical treatment methods |
Number of newborns |
|
Bypass gastrojejunostomy with Brown's anastomosis |
25 |
|
Duodenotomy |
24 |
|
End-to-end small intestine anastomosis |
4 |
|
Separation of congenital embryonic adhesions |
5 |
As can be seen from Table 1, in our studies, the most frequently used method for correcting congenital malformations of the GIT causing high intestinal obstruction was bypass gastrojejunostomy with a Brown anastomosis. In 1 (1.7%) newborn, the annular pancreas was combined with anal atresia, and a bypass gastrojejunostomy with a Brown's fistula and colostomy was performed (12). Five premature infants who were admitted on the 3rd and 7th days from the maternity hospital in extremely severe condition with exicosis and hemorrhagic complications were not operated because of the high risk of surgical intervention in an incurable condition and died during preoperative preparation.
In the postoperative period, independent bowel movements were usually observed on the 3rd–4th day. Enteral feeding was started at different times, based on the appearance of peristaltic sounds, restoration of passage through the anastomosis, and a decrease in the volume of stagnant secretions through the gastric tube. In most cases, this occurred on the 10th –12th day. Two newborns developed gastrointestinal failure and received parenteral nutrition for 3 months, but subsequently developed multiple organ failure, which led to death.
Discussion
Our study demonstrated that among newborns with congenital intestinal obstruction male sex prevailed, and 48% of them were premature newborns. The CHIO was represented by complete duodenal membrane, duodenal atresia, compression of the duodenum by the ring-shaped head of the pancreas, atresia of the initial section of the jejunum and embryonic adhesions that compressed the duodenum. The CHIO was associated with congenital heart defects and Down syndrome in 38% of patients.
The surgical treatment was successful in all patients, with restoration of bowel passage on 10th-12th day. The mortality observed in 2 (3.4%) patients 3 months after surgery due to gastrointestinal failure.
Our results are in agreement with previous studies (6, 8-11).
Study limitations
The main limitation is its descriptive and retrospective nature of the study. Further prospective studies are needed to explore long-term outcomes of surgery for CHIO in newborns.
Conclusions
The study allowed us to thoroughly examine issues related to surgical correction of congenital high intestinal obstruction in newborns. Analysis of clinical data showed that individual selection of surgical intervention tactics, taking into account the anatomical and physiological characteristics of the patient, timely diagnosis, and subjective postoperative management contribute to a reduction in the frequency of complications and mortality in the early postoperative period.
Thus, timely diagnosis of fetal malformations in the antenatal period allows determination of treatment tactics and improves postoperative outcomes.
High congenital intestinal obstruction in newborns requires the use of various types of surgical intervention on the gastrointestinal tract, and a well-established algorithm for surgical correction of a specific type of congenital intestinal obstruction will improve the treatment outcomes for newborns with this pathology. Optimizing surgical tactics for high congenital intestinal obstruction in newborns is an important area in neonatal surgery, contributing to improved long-term treatment outcomes.
Ethics: The informed consent parents or guardians of newborns for all procedure was obtained. The approval of Institutional Ethical Committee was not required for retrospective study.
Peer-review: External and internal
Conflict of interest: None to declare
Authorship: T.A.A., K.A.U., and N.F.G. equally contributed to the study and manuscript preparation and fulfilled authorship criteria.
Acknowledgements and funding: None to declare
Statement on A.I.-assisted technologies use: We declare that we did not use AI-assisted technologies in preparation of this manuscript
Availability of data and materials: Contact authors. Any data share should be conducted in frame of fair use, acknowledgement of data source and/collaboration
References
| 1.Zheleznov AC, Ermolaeva NS, Otdelnaya LA, Senina MS. Feature of congenital instestinal obstruction: Clinical-experimental study. Modern Probl of Scie Educ 2020; 1. Available at:URL: https://science-education.ru/ru/article/view?id=29565 https://doi.org/10.17513/spno.29565 |
||||
| 2.Choranova TA. Prediction of development of complications in newborns with congenital intestinal obstruction. Dissertation (candidate medical scinece). Rostov-on-Don. 2013. | ||||
| 3.Borsellino A, Zaccara A, Nahom A, Trucchi A, Aite L, Giorlandino C, et al. False-positive rate in prenatal diagnosis of surgical anomalies. J Pediatr Surg 2006; 41: 826-9. https://doi.org/10.1016/j.jpedsurg.2005.12.024 PMid:16567202 |
||||
| 4.Ergashev NSH, Sattarov JB. Diagnostics and treatment of congenital intestinal obstruction in newborns. Taskent. 2013. | ||||
| 5.Suman K, Shanbhag S, Joshi YM. Large amplitude oscillatory shear study of a colloidal gel near the critical state. J Chem Phys 2023; 158: 054907. doi: 10.1063/5.0129416. https://doi.org/10.1063/5.0129416 PMid:36754789 |
||||
| 6.Savvina VA, Varfolomeev AP, Ohlopkov ME, Nikolaev VN. Congenital intestinal obstruction: choice of surgical tactic and technique of surgery stitch. Russ Vestn Ped Surg Anesthesiol and Reanmatol 2012; 2: 69-73. | ||||
| 7.Best KE, Rankin J. Is duodenal atresia more common in Down Syndrome? Arch Dis Child Fetal Neonatal Ed 2016; 101: F169-74. doI: 10.1136/archdischild-2015-309827 | ||||
| 8. Patterson KN, Cruz S, Nwomeh BC, Diefenbach KA. Congenital duodenal obstruction - Advances in diagnosis, surgical management, and associated controversies. Semin Pediatr Surg 2022; 31: 151140 doi: 10.1016/j.sempedsurg.2022.151140 https://doi.org/10.1016/j.sempedsurg.2022.151140 PMid:35305801 |
||||
| 9. Parmentier B, Peycelon M, Muller CO, El Ghoneimi A, Bonnard A. Laparoscopic management of congenital duodenal atresia or stenosis: A single-center early experience. J Pediatr Surg 2015; 50: 1833-6. doi: 10.1016/j.jpedsurg.2015.05.007 https://doi.org/10.1016/j.jpedsurg.2015.05.007 PMid:26093906 |
||||
| 10. Mustafawi AR, Hassan ME. Congenital duodenal obstruction in children: a decade's experience. Eur J Pediatr Surg 2008; 18: 93-7. doi: 10.1055/s-2008-1038478 https://doi.org/10.1055/s-2008-1038478 PMid:18437652 |
||||
| 11.Escobar MA, Ladd AP, Grosfeld JL, West KW, Rescorla FJ, Scherer LR 3rd, et al. Duodenal atresia and stenosis: long-term follow-up over 30 years. J Pediatr Surg 2004; 39: 867-71. doi: 10.1016/j.jpedsurg.2004.02.025 https://doi.org/10.1016/j.jpedsurg.2004.02.025 PMid:15185215 |
||||
| 12. Uzakbaev KA, Akmentieva TA, Poroshai VN. Analysis of raise in congenital intestinal obstruction in newborns of Kyrgyzstan. Zdrav Kyrgyzstan 2023; 2: 22-7. doi.10.51350/zdravkg2023.2.6.3.22.27 | ||||
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

