Letter to the Editor: Severity of obstructive sleep apnea and its impact on coronary artery disease outcomes: A cross-sectional study in Egypt
LETTER TO THE EDITOR
Letter to the Editor: Severity of obstructive sleep apnea and its impact on coronary artery disease outcomes: A cross-sectional study in Egypt
Article Summary
- DOI: 10.24969/hvt.2025.591
- CARDIOVASCULAR DISEASES
- Published: 08/09/2025
- Received: 03/09/2025
- Accepted: 04/09/2025
- Views: 1621
- Downloads: 1284
- Keywords: STOP-BANG, sleep apnea, cardiovascular disease, screening tool, primary care
Address for Correspondence: Shirin Talapbek Kyzy, Peoples` Friendship University of Russia name after Patrice Lumumba (RUDN), Moscow, Russia
E-mail: shirin@gmail.com
Letter to the Editor
Letter to the Editor: Severity of obstructive sleep apnea and its impact on coronary artery disease outcomes: A cross-sectional study in Egypt
Key words: STOP-BANG, sleep apnea, cardiovascular disease, screening tool, primary care
Dear Editor,
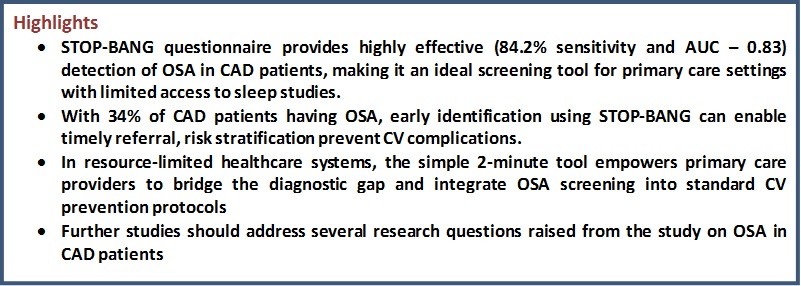
I read with great interest the recent study by Hossam Eldin M. Mahmoud et al. (1) assessing the prevalence of obstructive sleep apnea (OSA) among patients with coronary artery disease (CAD), its association with CAD severity and cardiac funct ion, and the diagnostic utility of the STOP-BANG questionnaire. As a pulmonologist, I commend the authors for their rigorous methodology and clinically significant findings, which reinforce the critical intersection between respiratory and cardiovascular (CV) health.
The study`s finding that 34% of CAD patients had OSA, with 24% exhibiting moderate-to-severe disease (AHI =15), aligns with growing evidence that OSA is not merely a comorbid condition but a notable contributor to CV morbidity. This prevalence is substantially higher than the general population (estimated at 10–17% in middle-aged adults), underscoring the need for routine OSA screening in cardiac clinics (2). The strong association between OSA and elevated Gensini scores—a quantitative measure of coronary atherosclerosis severity - further supports the role of chronic intermittent hypoxia, oxidative stress, and sympathetic overactivity in accelerating atherosclerotic progression (3).
Notably, the authors demonstrate that OSA is linked to both systolic and diastolic dysfunction, as evidenced by reduced left ventricular ejection fraction (LVEF), lower tricuspid annular plane systolic excursion (TAPSE), elevated pulmonary artery systolic pressure, and increased E/e’ ratio. These echocardiographic abnormalities suggest that OSA contributes not only to myocardial ischemia but also to ventricular remodeling and pulmonary hypertension—key determinants of long-term prognosis in CAD patients. The negative correlation between oxygen desaturation index and LVEF/TAPSE highlights the direct impact of nocturnal hypoxemia on right and left ventricular performance, consistent with prior studies showing that repetitive hypoxic episodes induce endothelial dysfunction and myocardial strain (4).
The study’s validation of the STOP-BANG questionnaire as a screening tool is particularly valuable for clinical practice.
With a sensitivity of 84.2% and specificity of 77.4% (AUC 0.83), STOP-BANG proves to be a reliable instrument for identifying high-risk patients who warrant formal polysomnography. This is crucial given the limited accessibility of sleep studies in many healthcare settings.
Importantly, the simplicity and brevity of the STOP-BANG tool make it ideally suited for primary care and outpatient settings, where time is limited and resources are constrained. In general practice, emergency departments, or rural clinics, where access to polysomnography is often delayed or unavailable, STOP-BANG offers a practical, evidence-based solution for early risk stratification. A quick 2-minute assessment during a routine visit can identify patients at high risk for OSA, enabling timely referral and preventing complications. This is particularly vital in low- and middle-income countries, where sleep laboratories are scarce, and undiagnosed OSA contributes significantly to the burden of CV disease. By empowering primary care providers with validated screening tools like STOP-BANG, we can bridge the diagnostic gap and ensure that high-risk patients are not overlooked simply due to systemic limitations.
However, while the STOP-BANG score >3.5 shows strong diagnostic performance, it should not replace objective sleep testing, especially in high-risk cardiac populations. Polysomnography remains the gold standard, and existing data suggest that treatment of OSA with continuous positive airway pressure improves CV outcomes, including blood pressure control, arrhythmia burden, and even mortality in patients with ischemic heart disease (5). Therefore, integrating sleep screening into standard CAD management protocols—like lipid or hypertension assessment—could significantly enhance secondary prevention strategies.
Nevertheless, these findings raise several important questions regarding the optimal use of the STOP-BANG questionnaire in clinical practice. How effective is the integration of this tool into routine primary care protocols, particularly in resource-limited settings? Can the threshold score of STOP-BANG be adjusted to enhance its predictive accuracy specifically in patients with established coronary artery disease? What is the sensitivity and specificity of the questionnaire across different subpopulations—such as women, older adults, or individuals with obesity—where the clinical presentation of OSA may differ? Furthermore, it remains to be explored to what extent the systematic use of STOP-BANG during initial patient assessment facilitates earlier diagnosis, reduces time to confirmatory testing, and ultimately improves CV outcomes. Addressing these questions could support a more targeted integration of OSA screening into the comprehensive management of patients with CAD.
In conclusion, this well-conducted study provides compelling evidence that OSA is highly prevalent in CAD patients and independently associated with worse cardiac structure and function. It reinforces the importance of a multidisciplinary approach involving cardiologists, pulmonologists, and sleep specialists. Raising awareness among clinicians and patients alike could transform outcomes in this high-risk population. As we continue to unravel the bidirectional relationship between sleep and heart health, proactive identification, and management of OSA may prove to be one of the most impactful yet underutilized strategies in modern cardiology.
Shirin Talapbek Kyzy
Peoples` Friendship University of Russia name after Patrice Lumumba (RUDN), Moscow, Russia
Peer-review: Internal
Conflict of interest: None to declare
Authorship: Sh,T.k.
Acknowledgements and Funding: None to declare
Statement on A.I.-assisted technologies use: Author declared they did not use AI-assisted technologies in reparation of this manuscript
Availability of data and materials: Do not apply
References
| 1. Mahmoud HEM, Hussein A, Taha EA, Dongol EM, Bakry AG. Severity of obstructive sleep apnea and its impact on coronary artery disease outcomes: A cross-sectional study in Egypt. Heart Vessels Transplant 2025: 9: 180-9. doi: 10.24969/hvt.2025.564 https://doi.org/10.24969/hvt.2025.564 |
||||
| 2.Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol 2013; 177: 1006-14. Doi: 10.1093/aje/kws342 https://doi.org/10.1093/aje/kws342 PMid:23589584 PMCid:PMC3639722 |
||||
| 3.Pack AI, Gislason T. Obstructive sleep apnea and cardiovascular disease: a perspective and future directions. Prog Cardiovasc Dis 2009; 51: 434-51. Doi: 10.1016/j.pcad.2009.01.002 https://doi.org/10.1016/j.pcad.2009.01.002 PMid:19249449 |
||||
| 4.Marin JM, Carrizo SJ, Vicente E, Agusti AG. Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with and without treatment with continuous positive airway pressure: observational study. Lancet 2005; 365: 1046-53. doi:10.1016/S0140-6736(05)71144-3 https://doi.org/10.1016/S0140-6736(05)71141-7 PMid:15781100 |
||||
| 5.McEvoy RD, Antic NA, Heeley E. CPAP for prevention of cardiovascular events in obstructive sleep apnea. N Engl J Med 2016; 375: 919-31. doi:10.1056/NEJMoa1606599 https://doi.org/10.1056/NEJMoa1606599 PMid:27571048 |
||||
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

