The heart-mind connection: Why the new ESC guidelines are a game-changer
EDITORIALS
The heart-mind connection: Why the new ESC guidelines are a game-changer
Article Summary
- DOI: 10.24969/hvt.2025.604
- CARDIOVASCULAR DISEASES
- Published: 04/11/2025
- Received: 27/10/2025
- Accepted: 27/10/2025
- Views: 1632
- Downloads: 768
- Keywords: Cardiovascular disease, mental health, psychosocial factors, management, guidelines
Address for Correspondence: Anna Mierzynska, Department of Cardiac Surgery, Department of Cardiology and Internal Diseases, Military Institute of Medicine - National Research Institute, Warsaw, Poland
E-mail: amierzynska@wim.mil.pl
ORCID: 0000-0002-7464-2343
Twitter (X): https://x.com/AnMiu123 Facebook: https://www.facebook.com/anna.mierzynska.90
Anna Mierzynska*
Department of Cardiac Surgery, Department of Cardiology and Internal Diseases, Military Institute of Medicine - National Research Institute, Warsaw, Poland
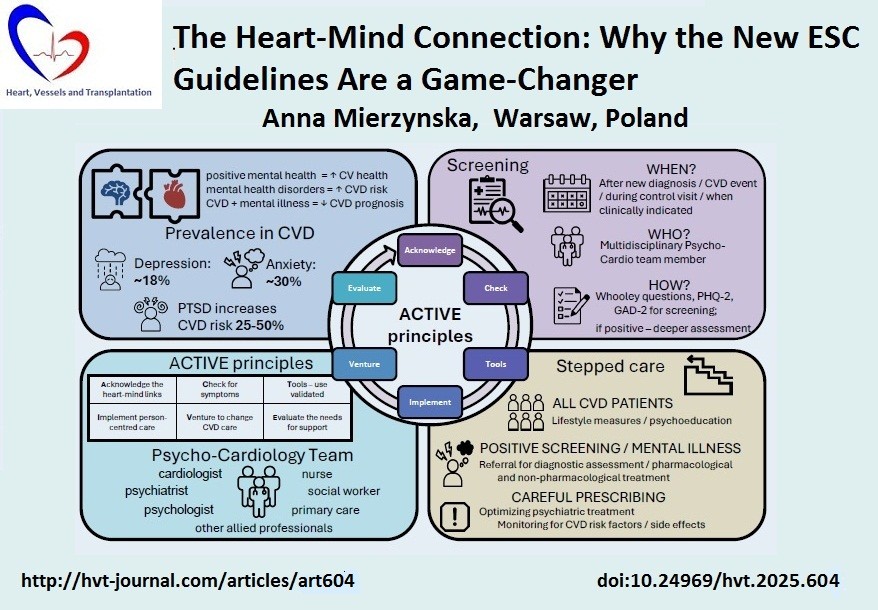
Graphical abstract
Key words: Cardiovascular disease, mental health, psychosocial factors, management, guidelines
During the European Society of Cardiology (ESC) Congress of this year, new guidelines were announced in several clinically relevant areas, including the consensus statement on mental health and cardiovascular disease (CVD) (1). Issues related to mental health, psychosocial factors, and access to psychological support have been present in the guidelines and other ESC documents for some time, showing how awareness of the importance of these topics for cardiac health is increasing (2, 3). This new document responds to the growing need to structure current knowledge and propose consistent methods of diagnosis, treatment, and care of mental health disorders in the context of CVD. The consensus statement addresses key issues related to the relationship between mental health and cardiovascular health, proposing methods and protocols for screening, diagnosis, and pharmacological and non-pharmacological interventions, with an emphasis on multidisciplinary care. An important aspect of this document is that patients from the ESC Patient Forum participated in its creation, and it includes clinical cases and patient perspectives, which is an important additional element that puts into practice certain principles and values shaping the document.
Mental health is an integral part of overall human health. It enables people to cope with life's stresses, fulfil their potential and goals, learn and work efficiently, and contribute to the development of their communities. This document adopts a perspective in which mental health is understood as a continuum from optimal health through symptoms and difficulties in this area to disorders, including severe mental illness, such as schizophrenia or bipolar disorder. The multidirectional relationship between mental and cardiovascular health has been proven by many studies, with evidence that positive mental health characteristics (e.g., positive personality traits or social support) are associated with better cardiac health, while mental health disorders increase the risk of CVD (4, 5). Moreover, cardiovascular events and chronic CVD affect mental health, exacerbating pre-existing mental illness and causing new ones. Additionally, the co-occurrence of CVD and mental illness can interact, worsening both mental health and the prognosis for CVD.
The consensus outlines three pillars of proper care for both areas: multidisciplinary action in the form of a psycho-cardiology team, a stepped care approach, and the principles contained in the acronym ACTIVE. A key element is the recognition that cardiac care specialists should collaborate with mental health specialists to ensure optimal care and treatment outcomes. Access to mental health care can vary, but ideally a multidisciplinary cardiology team should include a mental health specialist, a psychiatrist, or a psychologist to provide guidance on appropriate care and support for patients with CVD and their caregivers. Using telemedicine and online resources can help bridge gaps in mental health support where specialist resources are scarce.
According to ACTIVE principles, shifting routine clinical care towards a more person-centered approach requires: acknowledging (A) the multidirectional link between mental and cardiac health. Secondly, the presence of symptoms of mental health disorders should be systematically checked (C) during cardiology consultations, and cardiovascular risk factors should be checked during psychiatric consultations. Thirdly, validated tools (T) should be used to assess the mental health of people with CVD. Fourthly, practices based on shared decision-making and a stepped approach to care tailored to the individual should be implemented (I), considering also the importance of caregivers and their health and needs. Fifthly, medical specialists should venture (V) to change cardiovascular care by implementing the necessary adjustments. Sixthly, the current state of routine cardiovascular care in each setting should be evaluated (E), as well as the needs for organizational, educational, and clinical support necessary to implement the required changes.
Research on psychosocial factors affecting cardiac health is primarily focused on risk factors, mainly related to stress arising from work or financial situations, or negative life experiences. Nevertheless, we should not overlook the cardioprotective effect of positive factors, such as life satisfaction and positive emotions. Stress, described as the main psychosocial risk factor, has a negative impact on quality of life and the outcome of cardiac treatment. It increases the risk of developing symptoms of heart disease and worsens the condition of cardiac patients, influencing their prognosis. Therefore, interventions aimed at psychosocial problems or mental disorders should be implemented at the individual level, in the patient's environment, and in health policy.
The consensus statement focuses largely on three important mental health disorders, namely depression, anxiety disorders, and post-traumatic stress disorder (PTSD).
The findings of studies in this area are consistent, indicating that depression, prevalent in approximately 18% CVD patients, significantly worsens cardiac prognosis. High level of anxiety and anxiety disorders, diagnosed in 28.9% - 32.9% CVD patients, can affect their quality of life and adaptation to treatment, and the presence of PTSD can increase the risk of CVD by 25-50%. All those disorders influence cardiovascular health by physiological (e.g., HPA axis activation) and behavioral mechanisms (such as sedentary lifestyle or smoking) (6, 7).
The need for a practical approach to the diagnosis and treatment of mental health disorders was met by answering three basic questions referring to the moment of diagnosis, the person responsible for screening, and the choice of diagnostic tools.
The consensus suggests that screening should be carried out at specific times, for example, after a new diagnosis has been made, after the patient's condition has deteriorated, or during follow-up visits, at least once per year. Such screening can be performed by any member of the psycho-cardiology team who has the appropriate skills. To facilitate diagnostic decisions, the document proposes tools that will be helpful in conducting the screening assessment for anxiety or depression- simple, short, and with good diagnostic properties (Whooley questions, PHQ-2, GAD-2) (8-9). If it confirms the presence of symptoms of mental disorders, the assessment should be deepened by a mental health professional, and the information about the diagnosis should be communicated to the patient so that further steps can be taken regarding care.
Since mental health and mental disorders are on a continuum, the stepwise care is reasonable, i.e., intensification of intervention in response to the level of difficulties observed in patients, meaning that as symptoms of disorders become more severe, the involvement of the psycho-cardiology team in patient care should increase.
However, it is emphasized in the consensus that lifestyle interventions and psychoeducation should be directed at all cardiology patients, as they are beneficial for mental and cardiac health. Several non-pharmacological interventions are proven to be effective in cardiovascular care, with the impact on health-related quality of life, occurrence of cardiovascular events, and mortality; therefore, stress management, social prescribing, and other psychological interventions should be included in care (10, 11). The consensus also addresses the importance of motivational dialogue skills and the use of cardiac rehabilitation as a form of treatment that addresses various patients’ needs.
There is no consistent data on effectiveness and safety of psychiatric treatment in cardiac patients; therefore it is crucial to carefully consider the need for pharmacological interventions, focusing on possible drug interactions and adverse effects, especially in patients with heart failure or ventricular arrhythmias. Although antidepressants or anxiolytics can help increase psychosocial functioning and improve quality of life, it is important to remember that there is a tendency to overuse some types of medications (anxiolytic, sedative, and hypnotic) in the general population. Therefore, it is crucial in caring for CVD patients with mental disorders to monitor treatment and take precaution measures (e.g., regularly performing electrocardiogram) to optimize pharmacotherapy, and minimize potential drug interactions and side effects. This is especially vital for patients with severe mental disorders, knowing that antipsychotics can have side effects that influence the cardiovascular system, e.g., causing weight gain, dyslipidemia, hyperglycemia, or increasing the risk of arrhythmias. To enable proper monitoring of pharmacological treatment ESC consensus provides information on possible side effects of different antipsychotics and the source of current knowledge on the subject (https://www.crediblemeds.org/) (12).
Taking into consideration changes in the global social and economic situation, it is important to remember the psychosocial needs of various groups of people and their possible impact on their cardiovascular health. In modern societies, it is vital to emphasize the need for multidisciplinary collaboration in care for the elderly, as well as the differences in risk factors and illness trajectories related to gender, and the psychosocial situation of immigrants with its impact on cardiovascular risk. Current medicine also needs to embrace the unique situation of the growing population of cardio-oncology patients with their struggles with mental health, along with treatment for cancer and CVD. The ESC consensus sheds light on those special populations and encourages a broader view of cardiac treatment based on a comprehensive approach to patients’ health and their needs.
This is precisely what integrated care is all about: it allows for regular screening for psychopathological symptoms in order to minimize their impact on patients' cardiac health, to ensure proper care, and also suggests appropriate steps related to diagnosis and pharmacological and non-pharmacological interventions that will allow for the best possible integrated care for patients with both types of conditions. This is a groundbreaking document that offers an opportunity to change the way care is organized for people with special needs.
Peer-review: Internal
Conflict of interest: None to declare
Authorship: A.M.
Acknowledgement and funding: None to declare
Statement on A.I.-assisted technologies use: The author did not use AI-assisted technologies in preparation of this manuscript
Data and material availability: Does not apply
References
| 1.Bueno H, Deaton C, Farrero M, Forsyth F, Braunschweig F, Buccheri S, et al; ESC Scientific Document Group. 2025 ESC Clinical Consensus Statement on mental health and cardiovascular disease: developed under the auspices of the ESC Clinical Practice Guidelines Committee. Eur Heart J 2025: ehaf191. doi: 10.1093/eurheartj/ehaf191 https://doi.org/10.1093/eurheartj/ehaf191 PMid:40878270 |
||||
| 2.Visseren FLJ, Mach F, Smulders YM, Carballo D, Koskinas KC, Bäck M, et al; ESC National Cardiac Societies; ESC Scientific Document Group. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J 2021; 42: 3227-337. doi: 10.1093/eurheartj/ehab484 https://doi.org/10.1093/eurheartj/ehab484 PMid:34458905 |
||||
| 3.McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, et al; ESC Scientific Document Group. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: Developed by the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). With the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail 2022; 24: 4-131. doi: 10.1002/ejhf.2333 https://doi.org/10.1002/ejhf.2333 PMid:35083827 |
||||
| 4.Kubzansky LD, Huffman JC, Boehm JK, Hernandez R, Kim ES, Koga HK, et al. Positive psychological well-being and cardiovascular disease: JACC Health Promotion Series J Am Coll Cardiol 2018; 72: 1382-96. doi: 10.1016/j.jacc.2018.07.042 https://doi.org/10.1016/j.jacc.2018.07.042 PMid:30213332 PMCid:PMC6289282 |
||||
| 5.Vaccarino V, Prescott E, Shah AJ, Bremner JD, Raggi P, Dobiliene O, et al. Mental health disorders and their impact on cardiovascular health disparities. The Lancet Regional Health-Europe 2025; 56. https://doi.org/10.1016/j.lanepe.2025.101373 |
||||
| 6.Osborne MT, Shin LM, Mehta NN, Pitman RK, Fayad ZA, Tawakol A. Disentangling the links between psychosocial stress and cardiovascular disease. Circulation: Cardiovasc Imag 2020; 13: e010931 https://doi.org/10.1161/CIRCIMAGING.120.010931 PMid:32791843 PMCid:PMC7430065 |
||||
| 7.Ye S, Muntner P, Shimbo D, Judd SE, Richman J, Davidson KW, et al. Behavioral mechanisms, elevated depressive symptoms, and the risk for myocardial infarction or death in individuals with coronary heart disease: The REGARDS (Reason for Geographic and Racial Differences in Stroke) Study. J Am Coll Cardiol 2013; 61: 622-30. doi.org/10.1016/j.jacc.2012.09.058 https://doi.org/10.1016/j.jacc.2012.09.058 PMid:23290548 PMCid:PMC3568239 |
||||
| 8.Bosanquet K, Bailey D, Gilbody S, Harden M, Manea L, Nutbrown S, et al. Diagnostic accuracy of the Whooley questions for the identification of depression: a diagnostic meta-analysis. BMJ Open 2015; 5: e008913. doi: 10.1136/bmjopen-2015-008913 https://doi.org/10.1136/bmjopen-2015-008913 PMid:26656018 PMCid:PMC4679987 |
||||
| 9.Levis B, Sun Y, He C, Wu Y, Krishnan A, Bhandari PM, et al; Depression Screening Data (DEPRESSD) PHQ Collaboration; Accuracy of the PHQ-2 alone and in combination with the PHQ-9 for screening to detect major depression: Systematic review and meta-analysis. JAMA 2020; 323: 2290-300. doi: 10.1001/jama.2020.6504 https://doi.org/10.1001/jama.2020.6504 PMid:32515813 PMCid:PMC7284301 |
||||
| 10.Nie Y, Wang N, Chi M, Li A, Ji S, Zhu Z, et al.. Effects of psychological interventions on clinical outcomes in patients with cardiovascular diseases: A systematic review and meta-analysis. J Psychosom Res 2024; 187: 111938. doi: 10.1016/j.jpsychores.2024.111938 https://doi.org/10.1016/j.jpsychores.2024.111938 PMid:39321711 |
||||
| 11.Ski CF, Taylor RS, McGuigan K, Long L, Lambert JD, Richards SH, et al. Psychological interventions for depression and anxiety in patients with coronary heart disease, heart failure or atrial fibrillation. Cochrane Database Syst Rev 2024; 4: CD013508. doi: 10.1002/14651858.CD013508.pub3 https://doi.org/10.1002/14651858.CD013508.pub3 PMid:38577875 PMCid:PMC10996021 |
||||
| 12.De Hert M, Detraux J, van Winkel R, Yu W, Correll CU. Metabolic and cardiovascular adverse effects associated with antipsychotic drugs. Nat Rev Endocrinol 2011; 8 : 114-26. doi: 10.1038/nrendo.2011.156 https://doi.org/10.1038/nrendo.2011.156 PMid:22009159 |
||||
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

