Impact of resection vs respect techniques on left ventricular function after mitral valve repair: a systematic review
REVIEW
Impact of resection vs respect techniques on left ventricular function after mitral valve repair: a systematic review
Article Summary
- DOI: 10.24969/hvt.2025.605
- CARDIOVASCULAR DISEASES
- Published: 10/11/2025
- Received: 31/10/2025
- Accepted: 31/10/2025
- Views: 1143
- Downloads: 649
- Keywords: Mitral valve repair, left ventricular function, resection, respect, surgical repair
Address for Correspondence: Casey Christiany, Department of Thoracic, Cardiac, and Vascular Surgery, BP Batam Hospital, Batam, Riau Island, Indonesia
E-mail: caseychristiany03@gmail.com Phone: +6287884965742
ORCID: Casey Christiany - 0009-0001-1559-2147, Victor Jesron Nababan - 0009-0007-6973-6672,
Darma Satria - 0009-0008-0133-9184
Casey Christiany1, Victor Jesron Nababan1, Darma Satria2
1Department of Thoracic, Cardiac, and Vascular Surgery, BP Batam Hospital, Batam, Riau Island, Indonesia
21Department of Thoracic, Cardiac, and Vascular Surgery, Syiah Kuala University, Banda Aceh, Aceh, Indonesia
Abstract
Objective: Mitral valve disease, ranging from degenerative to infective origin, is one of the most prevalent left heart diseases globally and affects a large number of individuals. Conventionally, surgical repair has grown to become the treatment of choice, with two main techniques being resection and respect. Current literature has yet to address which technique is superior to the other, particularly in regard to left ventricular (LV) function.
Methods: We performed a systematic review and meta-analysis on three databases with a primary outcome of LV function alongside its’ parameters, and a secondary outcome of repair durability, mitral valve gradient, and mortality rates. Meta-analysis was performed using random effects, and results were displayed in forest plots. Risk of bias was conducted using the Newcastle-Ottawa Scale.
Results: Six retrospective studies were included, evaluating a total of 3376 patients. Pooled results showed that LV function were preserved equally in both groups, showing no statistically significant differences. The respect group had slightly lower mortality rates in comparison to the resect group, and the repair success rate showed a slight superiority in the respect group. Significant heterogeneity was observed on left atrial diameter (LAD) measurement, indicating variability. The overall differences in LV function coming from both techniques appear intangible. Plenty of consideration must be made beyond LV function in determining which repair technique should be performed on a patient.
Conclusion: This study demonstrated that both the resect and respect techniques were found to be equally excellent in preserving left ventricular function after mitral valve repair.
Key words: Mitral valve repair, left ventricular function, resection, respect, surgical repair
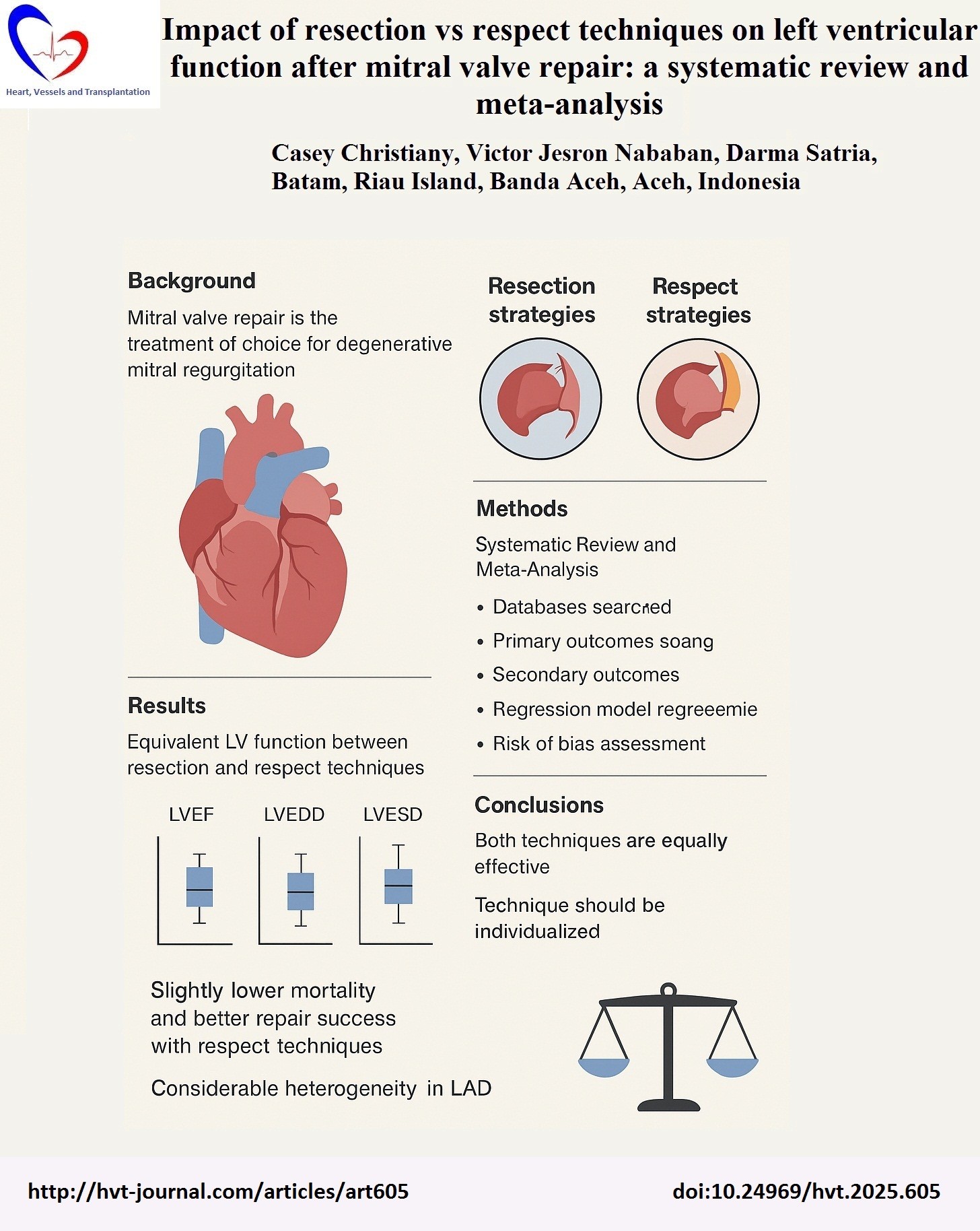
![]()
Graphical abstract
Introduction
Mitral valve disease remains as one of the most prevalent left heart valve diseases globally, with an incidence rising significantly as of recent (1). Developed nations, in particular, have experienced an increase in patients with degenerative mitral valve disease, and developing countries are still in the middle of battling against rheumatic heart diseases (2, 3). Among these diseases, mitral regurgitation (MR) is the most prominent pathology requiring surgical intervention, with recent studies estimating the prevalence of moderate-to-severe MR at 0.67%, and mitral valve prolapse (MVP) at 2.6% globally. These numbers, albeit small in percentages, make up a large number of individuals affected by significant mitral valve diseases (1, 4).
Conventionally, surgical repair has grown to become the treatment of choice for most patients with degenerative MR, with evidence proving better survival rates and long-term outcomes in comparison to mitral valve replacement (MVR) (5). In comparison to MVR, mitral valve repair has shown less operative risks; more ventricular function preserved, as well as reduced complications related to prosthetic valves. Current guidelines recommend surgical repair over replacement when feasible (5, 6).
Currently, two primary techniques are offered for mitral valve repair, being resection (or “resect”) technique, and the respect technique. The resect approach focuses on the excision of the diseased leaflet tissue, followed by the reconstruction of the remaining viable tissue (7, 8). On the other hand, the respect approach utilizes artificial neochordaes to re-suspend prolapsed leaflet segments, which is aimed to preserve the leaflet anatomy and structure. Ultimately, both techniques aim to restore valve competence and durability, however, their repercussions on valve function and clinical outcomes, such as left ventricular (LV) performance, remains unknown (9). Studies have found contrasting answers, with one study stating how the respect approach is a better modality in comparison to the former in terms of permanent pacemaker implantation rates and mean gradients (10), and other studies asserting how the resect approach is more reproducible and therefore are more commonly used (11). Other trials have also remained inconclusive (12, 13).
Current literature has yet to address the consequences or improvements of these techniques to the LV function, durability, and patient outcomes.
This systematic review and meta-analysis aim to bridge literature gaps and directly compare the resection versus respect techniques in mitral valve repair, focusing on their impact on left ventricular function, as well as other clinical outcomes.
Methods
This study is a systematic review and meta-analysis performed based on the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) 2020 guidelines (14). Our population included adult patients, categorized as individuals aged 18 and above undergoing mitral valve repair, with or without degenerative mitral valve disease, including stenosis and regurgitation. The intervention we chose to proceed with was the resecting technique, in comparison to the respecting technique. This study has two outcomes, with the primary outcome being changes in LV function, including left ventricular ejection fraction (LVEF), left ventricular end systolic diameter (LVESD), and left ventricular end diastolic diameter (LVEDD) after surgery. Our secondary outcome includes durability of repair, mitral valve gradient, and mortality rates after repair.
Literature searching was systematically performed in three databases up until July 29, 2025, including PubMed, Science Direct, and Google Scholar, with keywords tailored to each site as seen in Table 1. The general search terms included “Mitral Valve Repair”,” Resecting technique OR Resection technique”, and “Left Ventricular Function OR LVEF OR LVESD OR LVEDD”. We made use of available Boolean operators when necessary to narrow down or broaden results. Searching and screening were performed by two independent reviewers, with a third reviewer to mediate any discrepancies when needed.
Our inclusion criteria included articles published from the past 10 years (2015-2025), fit into our population, intervention, comparison, and outcomes, reporting at least one LV function parameter pre- and post-surgery, with a follow up duration of at least 3 months. Our exclusion criteria included case reports, MVRs, studies without a comparison group, and studies whose full texts are irretrievable.
The selected studies are then summarized into one table, with headings including but not limited to: (1) author; year of publication, (2) study design, (3) country of origin, (3) number of subjects included, (3) age (years, mean standard deviation), (4) patients’ characteristics, (5) mean follow-up duration, and (6) study findings.
|
Table 1. Searching Strategy |
||
|
Database |
Keywords |
Hits |
|
PubMed |
("mitral valve repair"[MeSH Terms] OR "mitral valve repair") AND ("resection technique" OR "resecting technique" OR "leaflet resection") AND ("respect technique" OR "respecting technique" OR "chordal replacement") AND ("left ventricular function" OR "LVEF" OR "LVESD" OR "LVEDD") |
9 |
|
Science Direct |
("mitral valve repair") AND ("resecting technique" OR "leaflet resection") AND ("respecting technique" OR "chordal replacement") AND ("left ventricular function" OR "LVEF" OR "LVESD" OR "LVEDD") |
37 |
|
Google Scholar |
("mitral valve repair") AND ("resecting technique" OR "leaflet resection") AND ("respecting technique" OR "chordal replacement") AND ("left ventricular function" OR "LVEF" OR "LVESD" OR "LVEDD") |
243 |
The article we selected discusses the resect and respect techniques. The resect technique is based on the principle of removing (resecting) the leaflet that has prolapsed or become redundant in order to restore the valve to its normal shape. Examples include quadrangular resection, triangular resection, and leaflet resection with sliding plasty. In the respect technique, the focus is on preserving all valve tissue without resection, repairing the prolapse using neochordae.
Pre- and post- data collected were then observed for both respect and resect groups respectively.
Statistical analysis
To determine effect sizes, a random effects model was performed, with results reported as pooled mean differences with a 95% confidence interval (CI). Heterogeneity was quantified through the I2 statistics, with a value of I2 of over 50% defined as considerable heterogeneity (15). Forest plots are displayed to visualize findings. All analyses were performed using Review Manager (RevMan 5.4). A p-value of 0.05 and below determines statistical significance.
A comprehensive risk of bias would also be performed on the studies using the Newcastle-Ottawa Scale (16), scrutinizing domains including the selection, comparability, and outcome of the studies. Similarly, two independent reviewers proceeded with the critical appraisal, and any disparities will be settled by a third reviewer.
Results
The PRISMA Flowchart for this study is shown in Figure 1. Our initial search yielded 289 records, with 18 duplicates removed before further screening. Overall, 184 records were then excluded further. We attempted to retrieve 87 studies; however, 76 studies were unable to be retrieved; hence, 11 studies were assessed for their eligibility. We further excluded 5 studies for the unavailability of their full texts and included 6 studies in this review (17–22).
Risk of bias assessment was performed using Newcastle-Ottawa Scale for Cohort studies with three studies showing overall very good risk of bias and three studies showing good risk of bias (Supplementary Table 1.). Three studies showed a participant selection bias.
Study characteristics
Tables 1 and 2 summarize the study characteristics and the main findings of the study. Six retrospective studies were included in this review, evaluating a total of 3376 patients who has undergone mitral valve repair with either resection or respect techniques. The studies were performed in either European countries (i.e., The Netherlands, Germany) or Asian countries (Singapore, Japan, China). The sample size of each study ranged from 72 to 2134 subjects, with mean ages ranging from 55.3 to 64 years old.
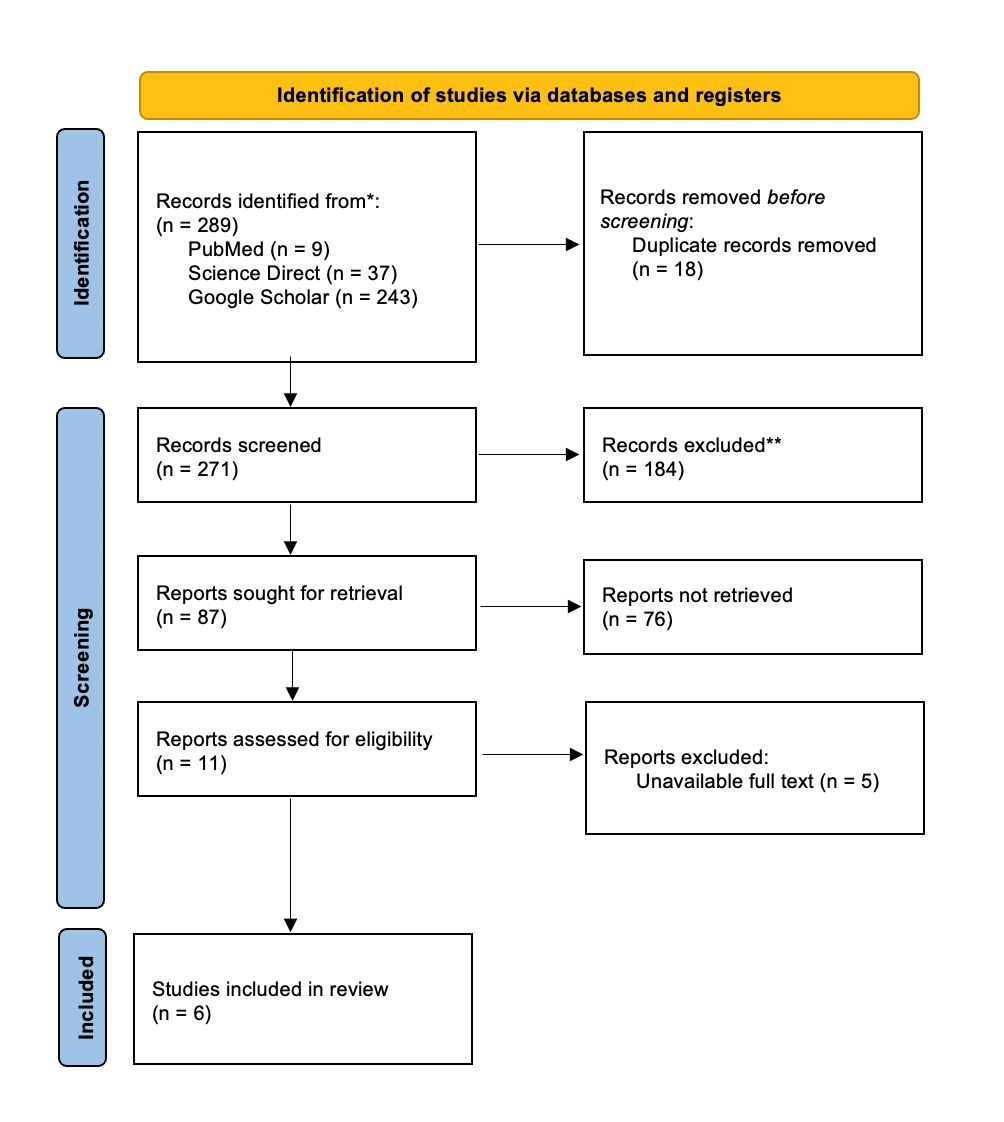
Figure 1. PRISMA Flowchart
Patients’ characteristics varied from having degenerative MR, to having an isolated posterior mitral leaflet (PML). The follow up duration varied from as short as one month, to as long as 87.6 months (17–22).
Generally, the LVEF was preserved in both groups over all of the included studies. The LVEF values ranged from 58 to 68 percent in both groups. Similar results were also seen in the left atrial diameter (LAD), LVEDD, and LVESD measurements. Ma et al. (18) showed nearly identical LAD values (44.37 mm in the Respect group, in comparison to 44.63 mm for Resection groups). This was also seen in the study performed by Wijngaarden et al., measuring 37mm for both groups (19).
Secondary outcomes are also shown in Table 2. Ma et al. (18) reported a low in-hospital mortality for both groups, with 1 patient (1.4%) for the respect group, and 0 patients (0%), whereas Cetinkaya et al. (17) showed a 0.4% mortality rate for the respect group and 1.9% mortality rate for the resect group. Imasaka et al. (20), on the other hand, observed no deaths throughout the study period. In terms of repair success rate, a 95.8% success rate in the respect group was observed by Cetinkaya et al. (17) in comparison to a 86.7% repair success rate for the resect group. Wijngaarden et al. (19) measured a mitral valve mean gradient, with the respect group having a mean gradient of 2.8 mmHg, and the resect group having a mean gradient of 2.9 mmHg.
|
Table 1. Summary of study characteristics |
||||||||
|---|---|---|---|---|---|---|---|---|
|
Study design |
Country |
No. of samples (Respect/ Resect) |
Age (years) |
Patients’ characteristics |
Mean follow-up (months) |
LVEF, % |
||
|
Respect |
Resect |
|||||||
|
Wijngaarden et al., 202219 |
Retrosp. cohort |
Netherlands |
125 (43/82) |
63 (12) |
Isolated PML, robotic repair |
42.0 (14.5) |
58 (7) |
57 (9) |
|
Ma et al., 202118 |
Retrosp. (matched) |
China |
317 (243/74) |
Respect: 55.3 (11) Resect: 55.8 (12) |
Degenerative MR, more multi-segment in Respect |
32 (median) |
67.86 (6.07) |
67.79 (5.51) |
|
Pfannmueller et al., 202121 |
Retrosp. |
Germany |
2134 (1751/383) |
Respect: 58.6 (12.4) Resect: 58.9 (13) |
Minimally invasive MV repair for MR |
73.2 (51.6) |
63.3 (8.6) |
63.8 (11.1) |
|
Cetinkaya et al., 201917 |
Retrosp. (propensity-matched) |
Germany |
526 (263/263) |
Respect: 61.8 (12.1) Resect: 62.1 (12.1) |
Isolated PML prolapse |
57.6 (respect) / 87.6 (resect) |
60.8 (7) |
61.5 (7.8) |
|
Chua et al., 201622 |
Retrosp. |
Singapore |
202 (98/104) |
Respect: 56.9 (10.9) Resect: 57.1 (12.1) |
Degenerative MR, isolated PML |
73.2 ( 48) |
63.7 (7.9) |
61.9 (7.9) |
|
Imasaka et al., 201520 |
Retrosp. |
Japan |
72 (30/42) |
Respect: 62 (15.1) Resect: 64 (11.3) |
Isolated PML prolapse |
1 |
62.9 (8.9) |
65.5 (9.9) |
|
LVEF – left ventricular rejection fraction, MR – mitral regurgitation, MV – mitral valve repair, PML – posterior mitral leaflet, rertrosp. – retrospective, SD –standard deviation |
||||||||
Visualized meta-analysis findings of this study in forest plots (Fig. 2). Overall, the pooled results of the meta-analysis showed the absence of statistically significant (overall effects: p>0.05) differences in left atrial or ventricular measurements (LAD, LVESD, LVEDD) and ejection fraction (LVEF) between the two groups. A significant heterogeneity is seen in the LAD measurement (I2= 80%), which indicates variability over the included studies.
Discussion
Findings of this systematic review and meta-analysis have shown that no differences were seen between the two techniques in preserving LV function. This is universally seen through the LAD size, LVEDD and LVESD measurements, as well as LVEF. In terms of the secondary outcomes, repair success rate was observed by one study (17), which showed a slight superiority of the respect group in comparison to the resect group.
|
Table 2. Summary of study results |
|||||||||
|---|---|---|---|---|---|---|---|---|---|
|
Author; year of publication |
LAD, mm (Mean (SD)) |
LVEDD, mm (Mean (SD)) |
LVESD, mm (Mean (SD)) |
LVEF, % (Mean (SD)) |
Other outcomes |
||||
|
Respect |
Resect |
Respect |
Resect |
Respect |
Resect |
Respect |
Resect |
||
|
Wijngaarden et al., 202219 |
37 (6) |
37 (8) |
51 (6) |
49 (8) |
33 (7) |
32 (7) |
58 (7) |
57 (9) |
MV mean gradient (mmHg): Respect: 2.8 (1.5) Resect: 2.9 (1.1) |
|
Ma et al., 202118 |
44.37 (6.93) |
44.63 (7.03) |
55.87 (6.10) |
55.99 (6.66) |
33.35 (4.84) |
34.47 (5.52) |
67.86 (6.07) |
67.79 (5.51) |
In-hospital mortality: Respect: 1 (1.4%) Resect: 0 (0%) |
|
Pfannmueller et al., 202121 |
NR |
NR |
NR |
NR |
NR |
NR |
63.3 (8.6) |
63.8 (11.1) |
NR |
|
Cetinkaya et al., 201917 |
54.8 (10.0) |
52.4 (10.2) |
55.0 (8.2) |
55.7 (6.7) |
34.3 (6.2) |
35.0 (6.2) |
60.8 (7) |
61.5 (7.8) |
Repair success rate: Respect: 252/263 (95.8%) Resect: 228/263 (86.7%) Mortality: Respect: 1/263 (0.4%) Resect: 5/263 (1.9%) |
|
Chua et al., 201622 |
48.8 (9.1) |
52.5 (9.6) |
56.0 (7.2) |
57.5 (7.2) |
33.4 (6.0) |
34.2 (5.5) |
63.7 (7.9) |
61.9 (7.9) |
NR |
|
Imasaka et al., 201520 |
NR |
NR |
57.8 (6.6) |
55.4 (7.2) |
35.5 (6.4) |
32.7 (7.0) |
62.9 (8.9) |
65.5 (9.9) |
No deaths observed |
|
LAD – left atrial dimension, LVEDD - left ventricular end-diastolic dimension, LVESD – left ventricular end-systolic dimension, MV – mitral valve, NR – not reported, SD – standard deviation |
|||||||||
However, this was the opposite for the mortality rate parameter, where the resect group had a slightly higher mortality rate. These parameters were not pooled; hence, we are unable to draw a conclusion for the secondary outcomes.
These findings demonstrate that both techniques were similarly capable of producing excellent LV outcomes, which is well supported by recent meta-analyses, illustrating that both methods lead to similar rates of long-term mortality, recurrence, and need of repeat surgeries, after adjusting for patients’ individual risk factors (13). Additionally, previous matched cohort studies have suggested that both approaches are associated with high survival rates, durable repair, as well as reverse remodeling of the left-ventricle. The same study, however, mentioned that a smaller LVEDD was seen among the respect group in comparison to the resect group (23). A different study has also seen a higher postoperative LVEF among patients who had undergone the respect technique (24). Regardless, the overall differences in functional recovery coming from both techniques appear intangible; hence, ultimately, the safety and efficacy of either approach are equally robust.
In order to effectively select the most appropriate repair technique, plenty of consideration must be made beyond LV function alone. This includes anatomical architecture, surgeon’s capabilities, and valve pathology tailored to each patient. Given the indistinguishable long-term results, the decision to respect or resect should, overall, aim to achieve leaflet mobility with highest durability, in addition to patients’ personal preferences (10, 23).
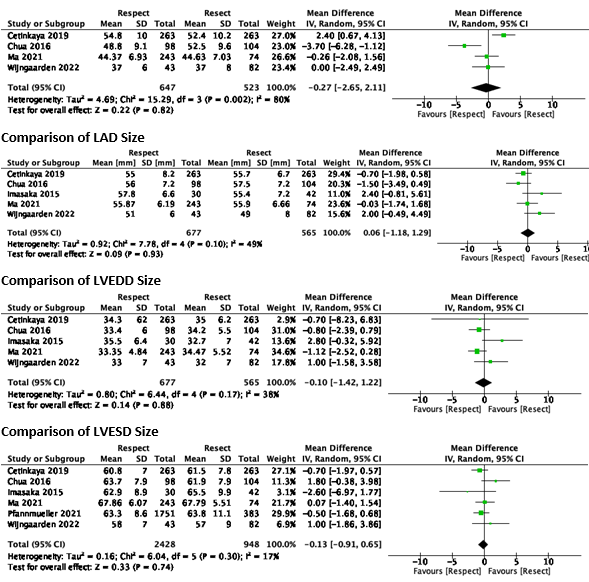
Figure 2. Forest plots on Resection vs Respect techniques on left ventricular function
LAD - left atrial dimension, LVEDD - left ventricular end-diastolic dimension, LVEF - left ventricular ejection fraction, LVEDD - left ventricular end-systolic dimension
Study limitations and directions for future research
This study has several strengths, including the inclusion of the most recent studies, as well as a specific focus on the objective parameters of LV function. However, this study does come with its’ limitations, including study heterogeneity, which may lead to inconsistent results.
Moreover, the studies included have slight differences in defining ‘resect’ and ‘respect’, which may also contribute to additional heterogeneity and variety among study methods. Furthermore, follow-up duration between studies were widely incongruous. A head-to-head randomized controlled trials with a longer follow-up duration may help establish a more uniformed study with less confounding and heterogeneity; hence, establishing a more credible and applicable finding. Additionally, comparing the measurement of longitudinal LV function, such as strain imaging, may also strengthen current findings.
Conclusion
This study demonstrated that both the resect and respect techniques were found to be equally excellent in preserving left ventricular function after mitral valve repair.
As this study primarily included retrospective studies, more prospective studies should be conducted to enhance the reliability of these findings.
Peer-review: External and internal
Conflict of interest: None to declare
Authorship: C.C., V.J.N., and D.S. equally contributed to the study and manuscript preparation, thus fulfilled authorship criteria
Acknowledgement and funding: None to declare
Statement on A.I.-assisted technologies use: The author s did not use AI-assisted technologies in preparation of this manuscript
Data and material availability: Does not apply
|
Supplementary table 1. Newcastle Ottawa scale for cohort studies |
||||||||||
|
Study |
Selection |
Compara- bility |
Outcome |
Total quality score |
AHRQ stan- dard |
|||||
|
Represen- tativeness of the EC |
Selection on the non-EC |
Ascer-tainment of the E |
Demonst- ration that OI was not present at start of study |
Compa-rability of subjects |
Assess- ment of outcome |
Adequate FU duration |
Adequacy of cohort FU |
|||
|
Wijngaarden et al., 202219 |
a(*) |
a(*) |
a(*) |
b(*) |
a(**) |
a(*) |
b(*) |
a(*) |
9 |
Very good |
|
Ma et al., 202118 |
a(*) |
c |
a(*) |
b(*) |
a(**) |
a(*) |
b(*) |
a(*) |
8 |
Good |
|
Pfannmueller et al., 202121 |
a(*) |
c |
a(*) |
b(*) |
a(**) |
a(*) |
b(*) |
a(*) |
8 |
Good |
|
Cetinkaya et al., 201917 |
a(*) |
a(*) |
a(*) |
b(*) |
a(**) |
a(*) |
b(*) |
a(*) |
9 |
Very good |
|
Chua et al., 201622 |
a(*) |
c |
a(*) |
b(*) |
a(**) |
a(*) |
b(*) |
a(*) |
8 |
Good |
|
Imasaka et al., 201520 |
a(*) |
a(*) |
a(*) |
b(*) |
a(**) |
a(*) |
b(*) |
a(*) |
9 |
Very good |
|
E- exposure, EC – exposed cohort, FU-follow-up, OI – outcome of interest |
||||||||||
References
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

