What is new in the 2025 ESC guidelines for the management of myocarditis and pericarditis?
EDITORIALS
What is new in the 2025 ESC guidelines for the management of myocarditis and pericarditis?
Article Summary
- DOI: 10.24969/hvt.2025.606
- CARDIOVASCULAR DISEASES
- Published: 16/11/2025
- Received: 31/10/2025
- Accepted: 31/10/2025
- Views: 3674
- Downloads: 725
- Keywords: Myocarditis, pericarditis, management, guidelines
Address for Correspondence: Adam Stanczyk, Medical University of Lodz, Lodz, Poland
E-mail: stanczykpl@yahoo.com
Adam Stanczyk
Medical University of Lodz, Lodz, Poland
Abstract
The European Society of Cardiology (ESC), in collaboration with Association for European Paediatric and Congenital Cardiology (AEPC) and the European Association for Cardio-Thoracic Surgery (EACTS), has published for the first time Integrated Guidelines for Myocarditis and Pericarditis. As part of the guidelines, a new term has been introduced - inflammatory myopericardial syndrome - IMPS. The aim was to increase clinical awareness of the full spectrum of this disease and to improve the diagnostic process. The guidelines set a new paradigm for management, highlighting the key role of multimodal imaging – with a particular focus on cardiac magnetic resonance imaging and the role of genetic testing. The document also contains detailed recommendations to help patients return to physical and professional activity more quickly.
Key words: Myocarditis, pericarditis, management, guidelines
What is new?
The Guidelines for the management of myocarditis and pericarditis, presented at the ESC Congress in Madrid, update and replace the previous version of the 2015 ESC Guidelines on pericarditis (1). Guidelines on pericarditis have been published twice before, while myocarditis was covered till now only in a consensus and states of the experts, but for the first time in a guidelines. Additionally this guidelines are endorsed by the Association for European Paediatric and Congenital Cardiology (AEPC) and the European Association for Cardio-Thoracic Surgery (EACTS).
The first most important information from these guidelines is the emergence of a new disease entity, which is inflammatory myopericardial syndrome (IMPS). Why did the authors of the guidelines decide to create such a term? This is due, among other things, to the anatomical continuity of the tissues that make up the heart muscle. It rarely happens that the inflammatory process is limited only to the heart muscle without covering a fragment of the pericardium and vice versa. The creation of such a disease is supported by radiological factors, which are extremely similar in both myocarditis and pericarditis. These guidelines provide a full spectrum of diagnoses between myocarditis and pericarditis. A new category – IMPS – was introduced as an umbrella term to better understand the potential overlap of myocarditis and pericarditis during the initial diagnostic process until the final diagnosis is made (Fig.1).
In addition, the timeframe has been defined very precisely and in detail. This means that acute inflammation of both the heart muscle and pericardium, it is a process that lasts up to 1 month. Chronic inflammation is a condition that lasts longer than 3 months. On the other hand, all states in between are subacute states. The current ESC guidelines set a new paradigm for management, highlighting the key role of multimodal imaging – with particular focus on cardiac magnetic resonance imaging – in the diagnosis of IMPS. The document also contains detailed recommendations to help patients return to physical and professional activity more quickly - often after prior additional tests assessing the safety of resuming activity.
The authors of the guidelines emphasize the important role of genetic testing in the diagnosis of IPMS. Of course, these tests should be performed in a special group of patients, i.e. in those patients who have a family history of cardiomyopathy or sudden cardiac death. The second group consists of patients with recurrent pericarditis or with current symptoms of other diseases that may suggest a genetic basis.
The authors of the guidelines point out that in the process of searching for an etiological agent, serological tests for viral infection should not be routinely performed, except in 3 cases, i.e. patients with hepatitis virus (HCV) infection, HIV infection or Lyme disease.
Graphical abstract
The guidelines reinforce the role of the gold standard in the non-invasive diagnosis of IMPS patients, which is magnetic resonance imaging. Attention is drawn to the fact that this examination should be performed at the initial moment, i.e. at the time of searching for and making a diagnosis, and should be repeated after 6 months. On the other hand, the gold standard confirming the diagnosis of myocarditis is endomyocardial biopsy.
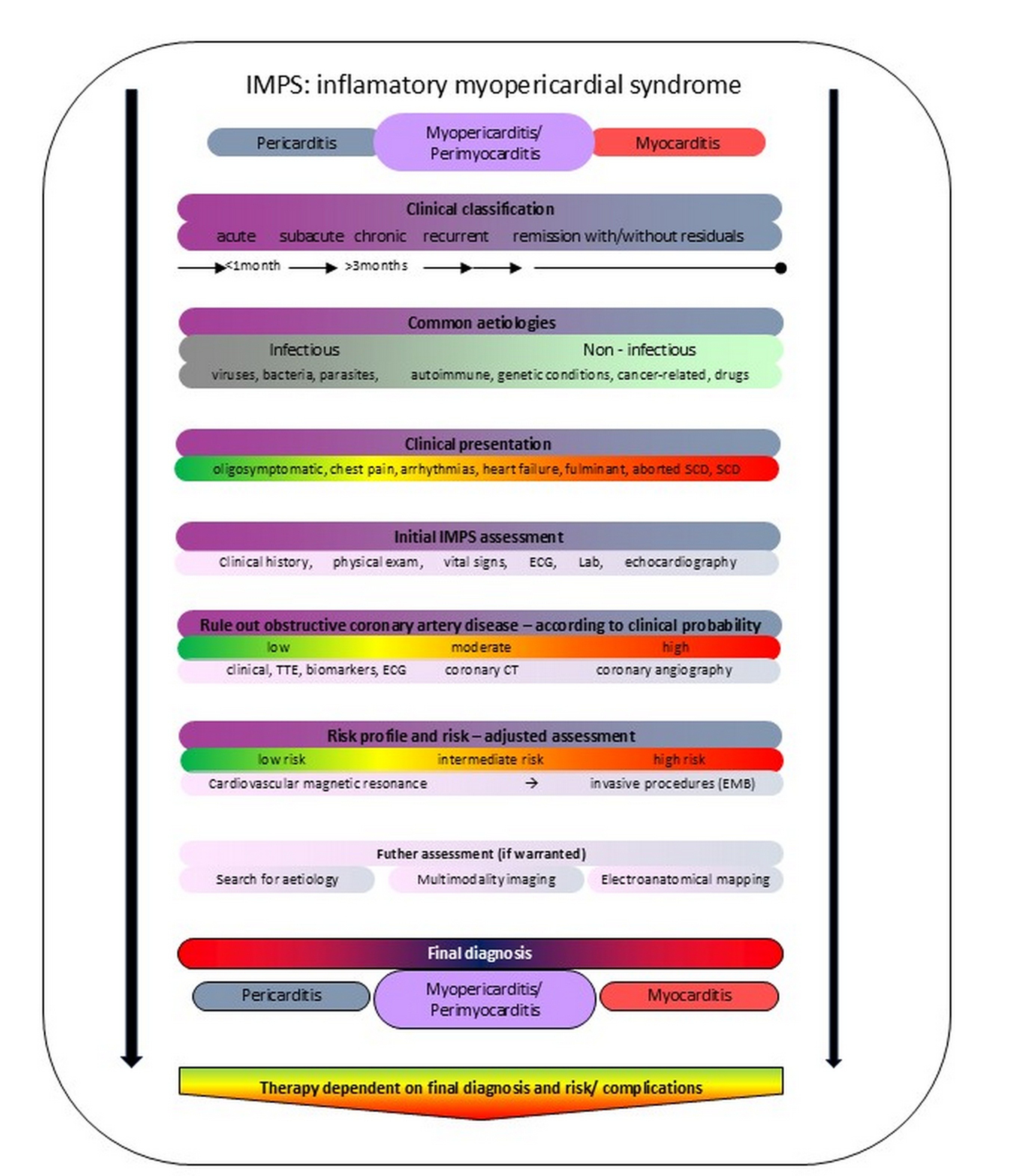
Figure 1. Inflammatory myopericardial syndrome
CT – computed tomography, ECG – electrocardiography, Lab – laboratory, SCD – sudden cardiac death, TTE – transthoracic echocardiography,
A biopsy is, of course, an invasive examination, associated with the risk of dangerous complications, so it should be performed in centers with a high degree of reference, by experienced cardiologists, of course, in order to minimize this risk risks, and it is also reserved for the most severe patients who are in cardiogenic shock and who do not respond to the treatment used in them. Polymerase chain reaction biopsy analysis for viral etiology is particularly valuable.
Each patient with both myocarditis and pericarditis is classified into 3 strictly defined risk groups: low, intermediate and high. On this basis, a decision is made about the possible need for hospitalization and the choice of therapy. A high-risk patient absolutely requires immediate hospitalization. A low or intermediate-risk patient may receive outpatient treatment. After a week, he should be re-evaluated for where he came from, in terms of risk and the need for hospitalization.
Another important piece of information indicated by the authors of the guidelines concerns personalized physical activity. Until now, the recommended rest period for patients with myocarditis was six months. Currently, this period of absolute abstention from physical exertion has been shortened to a month, then after performing additional tests, such as Holter electrocardiography, echocardiography, control of inflammatory parameters, markers of myocardial damage, and then we can consider returning to physical activity after performing an exercise test. Patients who have a severe course should not return to physical exertion so quickly. Of course, if myocarditis patients experience symptoms of heart failure, then that patient must be treated according to the ESC guidelines for heart failure, if the patient develops arrhythmias, of course, the inclusion of a beta-blocker can be considered, so it is an individualized procedure depending on the symptoms presented.
The guidelines indicate in which situations we turn on corticosteroids and in what doses. They also specify second- or third-line drugs. The ESC suggests that patients with recurrent life-threatening arrhythmias protect them with a defibrillation vest. It seems to be an ideal way for the patients to return to full fitness, to give time for the inflammatory process to subside. Therefore, we secure these patients with such a vest for a period of six months and then we re-evaluate them and decide whether the patient requires implantation of a cardioverter-defibrillator or not. When it comes to treating patients with pericarditis, the drugs of choice are aspirin or nonsteroidal anti-inflammatory drugs in combination with colchicine. Corticosteroids are reserved for patients who cannot take nonsteroidal anti-inflammatory drugs. On the other hand, if this first-line therapy does not work, we add corticosteroids to these 2 drugs. Ultimately, if this triple therapy does not work, then interleukin-1 (Il-1) antagonists are reserved for this group of patients. We must also bear in mind that a patient with pericarditis is a patient at risk of suffering from tamponade and, if confirmed, further targeted treatment, starting from pericardiocentesis, through surgical drainage to the creation of the connection between pericardium and pleura.
Current guidelines indicate that the condition for proper care of a patient with IPMS is the presence of a multidisciplinary team that will allow us to diagnose the disease and treat the patient appropriately based on individual risk factors and the course of the disease process.
Peer-review: Internal
Conflict of interest: None to declare
Authorship: A.S.
Acknowledgement and funding: None to declare
Statement on A.I.-assisted technologies use: The author did not use AI-assisted technologies in preparation of this manuscript
Data and material availability: Does not apply
References
- 1.2025 ESC Guidelines for the management of myocarditis and pericarditis. Eur Heart J 2025; 46: 3952–4041 doi.org: 10.1093/eurheartj/ehaf192
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

