A retrospective comparative analysis of trends of selected echocardiographic parameters in tricuspid valve repair with mitral valve replacement cases involving use of suture annuloplasty vs ring annuloplasty for tricuspid repair: A single-center study
ORIGINAL RESEARCH ARTICLE
A retrospective comparative analysis of trends of selected echocardiographic parameters in tricuspid valve repair with mitral valve replacement cases involving use of suture annuloplasty vs ring annuloplasty for tricuspid repair: A single-center study
Article Summary
- DOI: 10.24969/hvt.2025.612
- CARDIOVASCULAR DISEASES
- Published: 04/12/2025
- Received: 14/09/2025
- Revised: 04/11/2025
- Accepted: 05/11/2025
- Views: 1079
- Downloads: 644
- Keywords: Tricuspid valve repair, Kay’s suture annuloplasty, De Vega’s suture annuloplasty, ring annuloplasty, mitral valve replacement, left ventricular ejection fraction, tricuspid regurgitation maximal gradient, right ventricular systolic pressure
Address for Correspondence: Shobhit Mathur, Department of Cardiovascular and Thoracic surgery, U.N. Mehta Institute of Cardiology and Research Center, Ahmadabad, Gujarat, India
Email: mathur.1shobhit@gmail.com
ORCID: Shobhit Mathur - 0009-0005-8058-9875; Archit Patel - 0000-0003-2201-0042; Pratik Shah - 0000-0002-3428-1280
Shobhit Mathur, Archit Patel, Sunil Kumar T, Pratik Shah
Department of Cardiovascular and Thoracic surgery, U.N. Mehta Institute of Cardiology and Research Center, Ahmadabad, Gujarat, India
Abstract
Objective: Suture annuloplasty (SA) and ring annuloplasty (RA) are both used for tricuspid valve repair. Previously there have been studies comparing intra-op and post-op parameters and outcomes. Here we highlight the comparison of trends of selected echocardiographic parameters in mitral valve replacement (MVR) cases with tricuspid repair done.
Methods: In this retrospective study, 70 cases who underwent MVR with tricuspid repair from 2024-25 at our institute were selected. Two groups of 35 cases each were made as per the technique of tricuspid repair used (SA and RA). Three echocardiographic parameters –left ventricular ejection fraction/right ventricular systolic pressure (LVEF/ RVSP) and tricuspid regurgitation maximal gradient (TR G max) values were documented at pre-operative / post-operative and 6 months follow up in both groups to observe the trend of changes in these parameters.
Results: Baseline demographic characters were statistically comparable in both groups. Both the groups show non-significant results trends observed during preoperative, postoperative and follow-up period. However, RA when compared with SA showed significant improvement (p<0.0001) in LVEF, RVSP and TR G max which was observed from preoperative period to follow-up. Both SA and RA resulted in significant reduction of TR severity postoperatively (p<0.001). At follow-up, mild TR was observed in 68.6% of patients with SA and 82.9% with RA . Recurrence of moderate-to-severe TR was lower in the RA group (17.1%) compared to the SA group (31.4%). These findings suggest that RA provides more durable correction of tricuspid regurgitation than SA.
Conclusion: Despite having different tricuspid valve repair techniques used, post-operative left ventricular dysfunction is inevitable but there is improvement in RVSP and TR G max. Hence, we conclude that both the annuloplasty techniques (ring and suture) can be used with RA performing better in terms of observed trends of echocardiographic parameters and in providing more durable correction of tricuspid regurgitation grades.
Key words: Tricuspid valve repair, Kay’s suture annuloplasty, De Vega’s suture annuloplasty, ring annuloplasty, mitral valve replacement, left ventricular ejection fraction, tricuspid regurgitation maximal gradient, right ventricular systolic pressure
Introduction
Regurgitation is the commonest etiology for surgical repair of tricuspid valve. Classification of tricuspid regurgitation (TR) is like primary and secondary or functional TR (FTR - most commonly encountered). FTR is multifactorial resulting from maladaptive right ventricular remodeling secondary to pulmonary hypertension or from atrial fibrillation leading to dilation of the right atrium, tricuspid annulus and base of the right ventricle, with pathological TV coaptation. Two main types of FTR are: pulmonary hypertension-FTR and idiopathic-FTR, depending on whether ventricular or atrial respectively is the premium movens of the disease (1). ![]()
Graphical abstract
In summary, secondary TR entails functional TR which also has subtypes as atrial or ventricular.
Primary TR cannot be and should not be repaired as affection of multiple leaflets is there in the pathology. The aim of repair is decreasing annulus diameter that will increase coaptation of leaflets and afterload reduction of right ventricle. Important anatomic landmark is the presence of atrioventricular node and conducting system within the triangle of Koch (demarcated as base of septal leaflet, coronary sinus orifice and tendon of Todaro). Annulus is also related to base of the aortic valve, membranous interventricular septum, right coronary artery, fibrous body and lateral atrioventricular junction.
The various techniques for the tricuspid valve repair are - suture annuloplasty (SA) (Kay’s and De Vega’s); ring annuloplasty (RA) (size of the ring is typically decided by measuring the distance from the anteroseptal commissure to the posteroseptal commissure); Clover technique (Alfieri); other methods like repair of leaflets, chordal transposition or neochord and sliding papillary muscle repair; and transcatheter repair (off-label use of the edge-to-edge clip repair system) (2).
Moderate to severe TR affects approximately 3% to 6% of the general population. Prevalence is remarkably increased with left-sided valvular lesions, noticeably higher with heart failure irrespective of the fact that heart failure is with reduced ejection fraction or with preserved ejection fraction, where the range is from 10% to 23% (3). However, in patients with rheumatic heart diseases, functional TR was frequent and associated with adverse outcomes. The continuation of right ventricle and right atrium remodeling leads to progression of TR with time (4).
Currently established grades of TR are mild, moderate, significant/moderate-severe, severe, massive and torrential, and based on semi-quantitative parameters as vena contracta width, effective regurgitant orifice area, regurgitant volume, regurgitant fraction by 3D-echocardiography (magnetic resonance imaging) and 3D echocardiographic vena contract width (5).
The prevalence of secondary TR is increased in patients presenting with left-sided valvular heart disease. Initially studied for mitral valvular heart disease, it may also occur as a result of aortic valvular heart disease. Even after correction of left sided valvular lesions, persistent TR is associated with long-term fall in survival and functional capacity loss.
TR is sensitive to changes in loading conditions, annular dilatation and leaflet coaptation, rather than TR severity itself, would predict for the future development of TR and would serve as a therapeutic guide (6). Remodeling annuloplasty of tricuspid valve based on dilation has shown to preserve and improve functional status whatever be the TR grade. TV annular dilatation can even have marginal or no TR as sometimes severe TR appears in due course of time as it is an ongoing continuing disease process (7).
Tang et al. (8), in their work on tricuspid valve RA have concluded that RA is associated with increased survival and event-free survival. Sung Ho Shinn et al.(9), have covered the dispute regarding the comparison of effectiveness of tricuspid valve repair methods - prosthetic ring vs suture annuloplasty - in patients undergoing operation for primary mitral valve disease. The conclusion was that late survival and TV durability following concomitant TV repair during mitral valve surgery did not differ with the technique of TV repair used.
Also, the etiology of mitral disease did not affect postoperative changes in TR. Kisho et al. (10), in their work concluded that Kay annuloplasty and RA were effective in eliminating TR at 3 years postoperatively. Kay annuloplasty is a simple and inexpensive. All moderate‑to‑severe functional TR should be approached for tricuspid valve repair irrespective of the technique used.
We are here presenting our research which is an retrospective observational cohort study comparing the trends of selected echocardiographic parameters in tricuspid repair done with mitral valve replacement (MVR). The two repair techniques (suture annuloplasty and ring annuloplasty) will be compared in terms of the trends of echocardiographic parameters. The aim will be to arrive at a conclusion that which technique performs better for functional TR encountered with primarily MVR. Here we highlight the comparison of trends of selected echocardiographic parameters in MVR cases with tricuspid repair done.
Methods
Study design and population
The study was done in the Department of Cardiovascular and Thoracic Surgery at our institute. The design is a retrospective observational cohort study, which is a hospital record based study. This study was conducted in accordance with the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) guidelines.
Study population is comprised of 70 patients with primarily mitral valve pathology warranting MVR and operated between 2024 – 2025, whose records were reviewed in the study. All had associated secondary/ functional TR requiring tricuspid valve repair (SA/ RA): 35 cases were MVR operated with SA (De Vega or Kay’s) while the other 35 cases were MVR operated with RA of tricuspid valve.
Inclusion and Exclusion Criteria
All had associated secondary/ functional TR requiring tricuspid valve repair (SA/ RA Patients less than 18 and more than 65 years of age were excluded. Patients with associated aortic valve replacement, pulmonary valve intervention, atrial septal defect, ventricular septal defect, other congenital disease and coronary artery disease were excluded.
As this being a retrospective analysis of the surgical outcomes of the surgical technique, prior ethics committee approval was not taken. All the patients had consented for the surgery and our study being a retrospective study we have a waiver of individual consent of patient according to Institutional Ethics Committee.
Baseline variables
Routine pre-operative workup and preparation was done including clinical examination, laboratory testing, electrocardiography, chest X-RAY, and two-dimensional transthoracic echocardiography by consultant cardiologist. We collected the following baseline variables: demographic – age, sex; anthropometric – height, weight and BSA, echocardiographic – regurgitant, stenotic and mixed lesions, history of infective endocarditis, size of left atrium and : tricuspid annular systolic plane excursion (TAPSE); surgical – history of redo surgery, cardiopulmonary bypass (CBT) and aortic cross-clamp (ACCT) times and duration of hospital stay.
Surgical technique (11)
Kay procedure - In 1965 Kay et al. described, for the first time, a repair technique to treat secondary TR. Using a 1-0 silk suture (placed through the posterior leaflet and the commissures), the posterior leaflet is completely excluded, and a functional bicuspid valve is finally obtained. It is preferable to put other sutures to reinforce the first stitch. In addition, some variants (i.e., the positioning of some pledgets) could be performed.
De Vega procedure - proposed in 1972. This procedure consists of reducing the area of the tricuspid annulus and rapidly became the most popular technique for the treatment of annular dilatation. It is generally performed by two 2-0 Ti-cron or 4-0 polypropylene running parallel sutures (with 5–6 mm bites), starting on the postero-septal commissure, through the endocardium, and directed around the perimeter of the orifice in a counterclockwise direction reaching the antero-septal commissure. The other parallel suture is placed about 1–2 mm outside the previous one, and finally tied together.
Ring annuloplasty - The idea of a prosthetic ring to reinforce the tricuspid annulus was first introduced by Carpentier in 1971. Rigid or semi-rigid ring has been designed to fix the annulus during systole, restoring the physiologic geometry of the valve, while flexible ones may be used as well to reduce the annular dilatation, but failed to restore the 3D morphology. The right size of the ring is chosen by measuring the distance from the antero-septal to postero-septal commissures (i.e., the surface of the anterior leaflet) and the ring is then implanted using eight to ten 2-0 Ti-cron™ stitches starting posteriorly (at the midpoint of the septal leaflet) and then proceeding counterclockwise. The surgeon must pay attention during the placement of stitches not to damage the conduction system and to avoid the aortic root at the level of septal and anterior leaflet, respectively. The last stitch is placed above the antero-septal commissure, and the ring is finally parachuted and fixed.
Routine steps of surgery were followed including administration of the cardioplegic solution. Day 1 was the day of surgery. Bedside two-dimensional echocardiography (transthoracic) was performed by consultant cardiologist. Follow up of the patients was through outpatient department (OPD) visits and follow-up echocardiography was done by consultant cardiologist at sixth month visit. LVEF, RVSP and severity of TR was graded as mild/ moderate and severe along with maximal gradient (G max) for TR were recorded in all three stages - pre-operative, post-operative, and six month follow-up.
Echocardiography
Left ventricular ejection fraction (LVEF) is the primary echocardiographic parameter for measurement of the chamber systolic function. LVEF (%) among the male population: 52% to 72% normal range; 41% to 51 mildly abnormal; 30% to 40% moderately abnormal; less than 30% severely abnormal; and LVEF (%) among the female population: 54% to 74% normal range; 41% to 53 mildly abnormal; 30% to 40% moderately abnormal; less than 30% severely abnormal (12).
Pulmonary hypertension is a routine finding in patients with heart failure. RVSP measurement can both confirm and assess its severity. Right ventricular systolic pressure (RVSP) has been associated with adverse outcomes. RVSP is classified as: normal (<40 mm Hg); severely elevated (≥60 mm Hg); moderately elevated (50-59 mm Hg); or mildly elevated (40-49 mm Hg) (13).
In TR, Doppler-estimated peak systolic tricuspid pressure gradient is the most reliable noninvasive method for evaluation of pulmonary artery systolic pressure. Value of >30 mm Hg is the upper normal limit (14).
Evaluation of echocardiographic parameters was done by the consultant cardiologist. For TR maximal pressure gradient (G max), continuous wave Doppler is put on TR jet and a graph is obtained. Then jet velocity is calculated and finally gradient is calculated. RVSP is calculated as right atrial pressure added to TR G max. For LVEF, in parasternal long axis view M- Mode is put on tip of mitral valve leaflets and internal diameters of LV at end systole and end diastole are measured and LVEF is calculated using modified Simpson’s rule method. This technique involves tracing the left ventricular endocardial border in both the apical four-chamber and apical two-chamber views during both end-diastole (maximum filling) and end-systole (minimum filling). The machine then calculates the end-systolic (ESV) and end-diastolic (EDV) volume at each stage using the formula: ![]() LVEF = ((EDV - ESV) / EDV x 100) to determine the LVEF. Standard Echocardiography machines were used in OPD - GE (s70 and VIVID IQ, Phillips) and in ICU GE (VIVID IQ) respectively.
LVEF = ((EDV - ESV) / EDV x 100) to determine the LVEF. Standard Echocardiography machines were used in OPD - GE (s70 and VIVID IQ, Phillips) and in ICU GE (VIVID IQ) respectively.
Statistical analysis
Data were analyzed using IBM SPSS (v26.0) machine. Chi-square and independent t-tests were used to compare categorical and continuous data between groups. Continuous data are expressed as mean (standard deviation), and categorical data as a number and a percentage. Heat map and bar graph was used for graphical representation. Any value of p<0.05 of considered as a statistical significance.
Results
The patient data are tabulated (Table -1) and plotted (Fig. 1). The demographic data, intra-op data and types of valve lesion (predominantly stenotic or regurgitant) were compared among both groups and p values were calculated as shown. It is clearly evident that data in both the groups are statistically comparable.
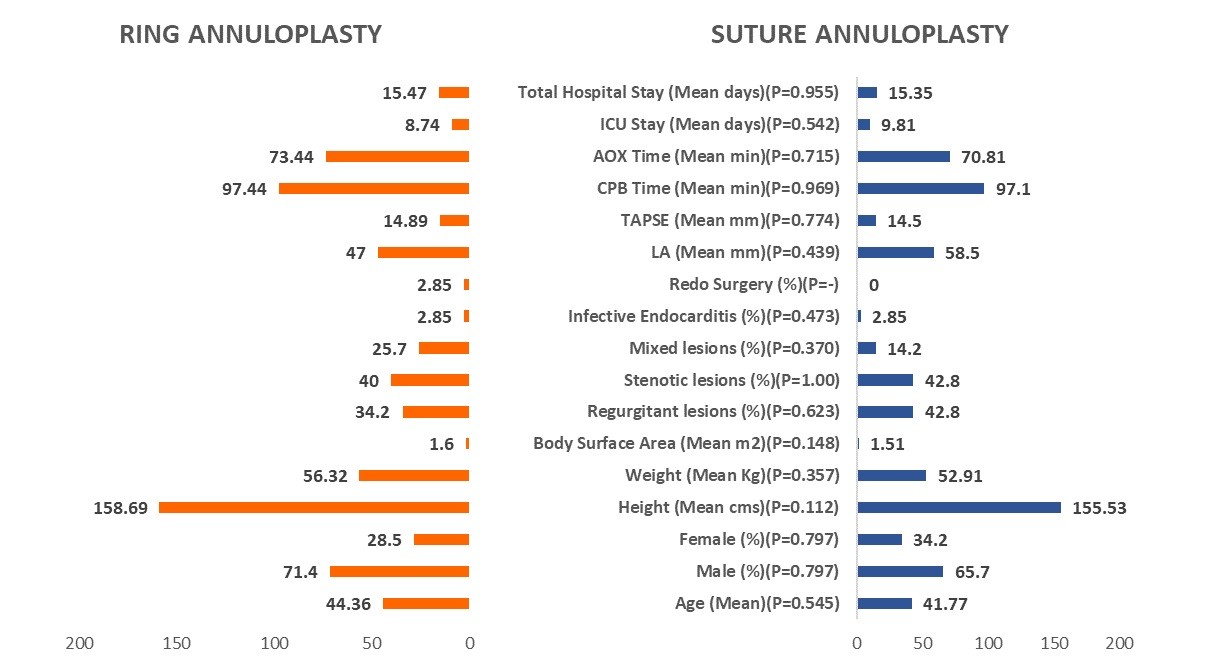
Figure 1. Patients` clinical characteristics
AOX - aortic cross-clamp, CPB - cardiopulmonary bypass, ICU - intensive care unit, LA -left atrium, TAPSE- tricuspid annular systolic plane excursion
|
Table 1. Clinical characteristics |
|||
|
Variables |
Suture Annuloplasty |
Ring Annuloplasty |
p |
|
Demographic |
|||
|
Age, years |
41.77 (15.48) |
44.36 (11.11) |
0.545 |
|
Male, n(%) |
23 (65.7) |
25(71.4) |
0.0629 |
|
Female, n(%) |
12(34.2) |
10(28.5) |
0.7968 |
|
Height, cm |
155.53 (9.15) |
158.69 (7.15) |
0.1120 |
|
Weight, kg |
52.91 (13.48) |
56.32 (9.04) |
0.357 |
|
Body surface area, kg/m2 |
1.51 (0.22) |
1.6 (0.15) |
0.148 |
|
Echocardiographic |
|||
|
Regurgitant lesions, n(%) |
15/35 (42.8) |
12/35 (34.2) |
0.6234 |
|
Stenotic lesions, n(%) |
15/35 (42.8) |
14/35 (40) |
1.000 |
|
Mixed lesions, n(%) |
05/35 (14.2) |
09/35 (25.7) |
0.3700 |
|
Infective endocarditis, n(%) |
01/35 (2.85) |
01/35 (2.85) |
0.4731 |
|
LA, mm |
58.5 (19.84) |
47 (14.53) |
0.439 |
|
TAPSE, mm |
14.5 (3.41) |
14.89 (3.18) |
0.774 |
|
Surgical |
|||
|
Redo surgery, n(%) |
00/35 (0) |
01/35(2.85) |
- |
|
CPB time, min |
97.1 (31.93) |
97.44 (20.26) |
0.969 |
|
ACCT, min |
70.81 (26.14) |
73.44 (18.59) |
0.715 |
|
ICU stay, days |
9.81 (5.33) |
8.74 (6.94) |
0.542 |
|
Total hospital stay, days |
15.35 (7.29) |
15.47 (7.35) |
0.955 |
|
Continuous data are represented as mean (SD). Categorical data represented as n(%). Significant p value is <0.05. Independent t test used for continuous data and Chi square test - for categorical data. ACCT - aortic cross-clamp time, CPB - cardiopulmonary bypass, ICU - intensive care unit, LA -left atrium, TAPSE- tricuspid annular systolic plane excursion |
|||
All the echocardiographic parameters are tabulated in Table – 2 for SA and RA groups. Mean pre-op values are taken as reference points, post-op and follow- up values are tabulated along with difference taking pre-op as reference value. Wherever there is a fall in values it has been depicted with a negative sign. A comparative p value has been recorded between the values of both groups to assess whether the difference in performance of both techniques of TV repair used is statistically significant or not.
There was no statistically significant difference in LVEF in the starting point of both groups (p>0.05).
|
Table 2. Echocardiographic parameters |
||||||
|
Variables |
Groups |
Pre-Op |
Post-Op |
Difference Pre-op as ref value |
Follow-up |
Difference Pre-op as ref value |
|
LVEF, % |
Suture Annuloplasty |
53.45 (7.48) |
45.03 (12.38) |
8.42 (4.9) |
45.39(10.7) |
4.18 (1.06) |
|
Ring Annuloplasty |
53.33 (6.85) |
46.34 (12.75) |
6.99 (5.9) |
49.27(8.54) |
7.94(3.85) |
|
|
p |
0.961 |
0.731 |
0.2739 |
0.201 |
< 0.0001 |
|
|
RVSP, mm Hg |
Suture Annuloplasty |
63 (17.98) |
35.49 (12.7) |
27.51 (5.28) |
30.36 (4.35) |
32.64 (13.63) |
|
Ring Annuloplasty |
68.75 (14.34) |
34.1 (5.53) |
34.65 (8.81) |
29.84 (4.41) |
38.91 (9.93) |
|
|
p |
0.592 |
0.743 |
0.0001 |
0.808 |
<0.0001 |
|
|
TR G max, mm Hg
|
Suture Annuloplasty |
43.6 (18.8) |
37.75 (22.84) |
5.85 (4.04) |
40.87(18.77) |
2.73 (0.03) |
|
Ring Annuloplasty |
46.2 (10.96) |
28.2 (12.46) |
18 (1.5) |
26.86(11.5) |
19.34 (0.54) |
|
|
p |
0.771 |
0.413 |
<0.0001 |
0.086 |
<0.0001 |
|
|
Continuous data are represented as mean (SD), significant p value is <0.05. Independent t test used for continuous data LVEF- left ventricular ejection fraction, pre-op- preoperative, post-op – postoperative, RVSP -right ventricular systolic pressure, TR G max - maximal tricuspid regurgitation gradient |
||||||
Both groups had LV dysfunction post-surgery but comparison of their LVEF values showed no difference (p>0.05). The absolute fall in LVEF from pre-op was -8.42 (4.9)% in SA group and -6.99 (5.9)% in RA group, dysfunction though seemingly more in SA group was not statistically significant. Both the groups recorded dysfunction during follow-up as LVEF recorded was 45.39 (10.7)% in SA group and 49.27 (8.54)% in RA group. Again, it was statistically not significant. The absolute fall in LVEF at follow-up was -7.94 (3.85)% in SA group and -4.18 (1.06)% in RA group. The absolute dysfunction is more pronounced in SA group as compared with RA group (p<0.0001).
Mean pre-op RVSP values did not differ between SA and RA groups (p>0.005). There was decrease in RVSP post-op in both groups without statistical significance when comparing the mean values, however the RVSP decline was significantly larger in RA group (p<0.0001). There were no difference in RVSP between SA and RA group on follow-up, however RVSP absolute decrease as compared reference level was more in RA group as compared with SA one (p<0.0001).
There were no differences between SA and RA groups in mean preoperative and postoperative TR Gmax values, as well as during follow-up (p>0.05 for all). Both groups displayed fall in TR G max values, however reduction was more pronounced in RA group as compared to SA group postoperatively and during follow-up (p<0.0001 for both).
Concisely, both suture and ring annuloplasty techniques resulted in improvement of RVSP and TR gradients postoperatively. RA demonstrated relatively better recovery of LVEF and greater reduction in TR gradient at follow-up. All parameters (LVEF, RVSP, TR Gmax) showed statistically significant improvement when compared to preoperative values at long-term follow-up (p<0.0001).
In Table 3, we have tabulated the grades of TR as mild/ moderate and severe in both the groups: SA and RA, and tried to analyze the trends of severity in pre/ post and follow up in both the groups to conclude which procedure gives better results. It is evident from analyzing the table that percentage of mild TR pre-op has gone up from nil in = pre-op in both groups to 68.57% in SA group and 82.86% in RA group during follow-up. The detailed of the above table can be easily understood by graphic visualization in Figure 2. We see that both groups cause adequate conversion from severe to mild but the performance in RA group is better.
|
Table 3. Echocardiographic grading of tricuspid regurgitation |
||||||
|
TR grade |
Suture Annuloplasty |
Ring Annuloplasty |
||||
|
Pre-Op |
Post-Op |
Follow-up |
Pre-Op |
Post-Op |
Follow-up |
|
|
Mild |
0/35 (0) |
25/35 (71.43) |
24/35 (68.57) |
0/35 (0) |
29/35 (82.86) |
29/35 (82.86) |
|
Moderate |
3/35 (8.57) |
6/35 (17.14) |
7/35 (20) |
4/35 (11.43) |
3/35 (8.57) |
4/35 (11.43) |
|
Severe |
32/35 (91.43) |
4/35 (11.43) |
4/35 (11.43) |
31/35 (88.57) |
3/35 (8.57) |
2/35 (5.71) |
|
Categorical data are represented as n(%) pre-op – preoperatively, post-op – postoperatively |
||||||
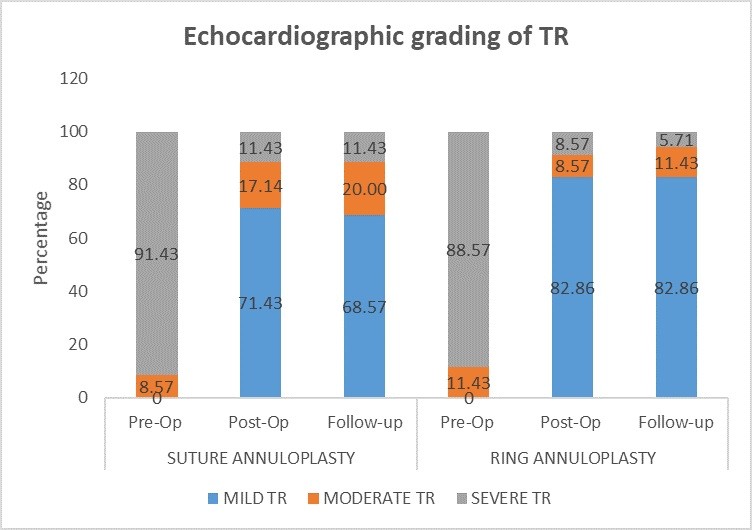
Figure 2. Severity of grades of TR in both groups
Pre-op – preoperatively, post-op – postoperatively, TR – tricuspid regurgitation
Further to arrive at a definite conclusion, we tabulate the percentages of severe TR and moderate TR in both groups in Table 4 and calculate the net change, which is expressed as a percentage.
|
Table 4. Trends of severity of tricuspid regurgitation in both groups |
||||||
|
TR |
Group |
Pre-op % |
Post-op % |
Follow-up % |
Net Change (Follow-up vs Pre-op) |
p |
|
Severe |
Suture Annuloplasty |
91.40% |
11.40% |
11.40% |
↓ 80% |
<0.0001 |
|
Ring Annuloplasty |
88.60% |
8.60% |
5.70% |
↓ 83% |
<0.0001 |
|
|
Moderate |
Suture Annuloplasty |
8.60% |
17.10% |
20% |
↑ +11.4% |
0.9 |
|
Ring Annuloplasty |
11.40% |
8.60% |
11.40% |
No change |
0.195 |
|
|
Categorical data represented as (%). Significant p value is < 0.05. Chi square test used |
||||||
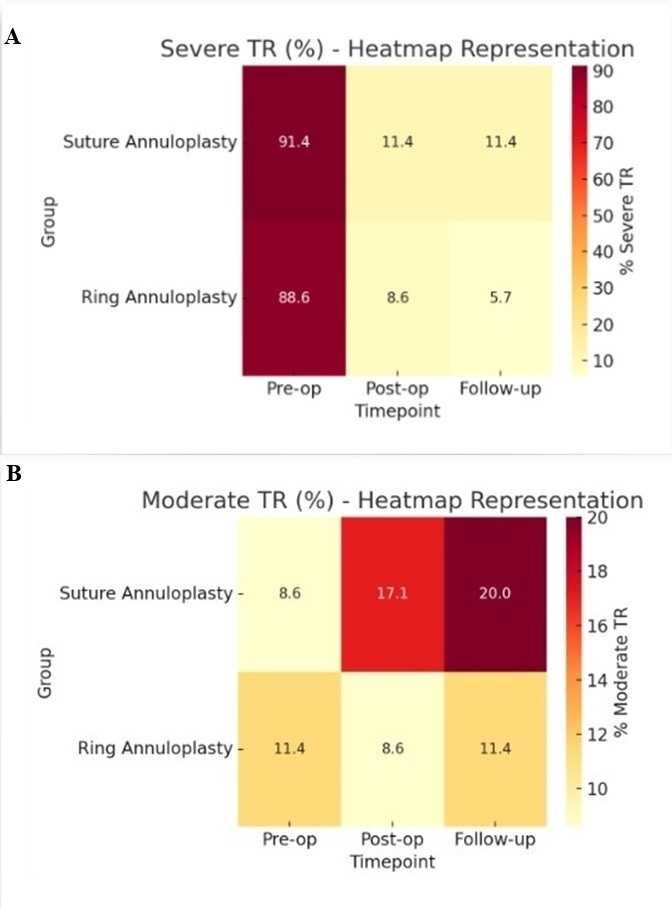
Figure 3. Heat map representation of trends of TR in both groups: A) severe TR B) moderate TR
Pre-op – preoperatively, post-op – postoperatively,
TR – tricuspid regurgitation
We can see that the percentage of severe TR declined from 91.4% to 11.4% in causing a net fall of 80% in SA group. This result is significant with a p value of <0.0001. On the other hand, the percentage of severe TR declined from 88.60% to 5.70% in causing a net fall of 83% in RA group. This result is significant with a p value of <0.0001.
It is evident that RA has performed better. The percentage of moderate TR increased from 8.6% to 20% with a net increase of 11.4%, which means that there were some cases, which after procedure could not be converted to mild TR. This change was not observed in RA group. Though these values are statistically non-significant but they point towards RA being a bit more superior than RA. For more eyes catching we are submitting a heat map representation diagram of severity grades of TR for both groups (Fig. 3).
Discussion
After a thorough discussion of the results in the above section, we can briefly summaries that baseline demographic characters were statistically non-significant in both groups. In postoperative period a statistically significant difference were found in LVEF/ RVSP and TRG Max in both groups when comparing to the respective preoperative values. However, the difference of these parameters between both groups came out statistically non-significant at pre-op, post op and at six months follow-up. The performance of RA was also better in terms of reduction of severe TR in post-op and follow-up periods.
Now, starting with our discussion there have been works on comparison of short and long-term results of SA vs RA of tricuspid valve. For example, Turkmen et al. (15) compared de Vega’s vs Kay’s annuloplasty vs flexible vs semirigid annuloplasty and concluded that RA is superior when it comes to reducing systemic pulmonary hypertension, TR regression and improvement in NYHA class in functional TR repairs. Kisho et al (10), concluded that annuloplasty (Kay’s and ring) was effective in eliminating TR at 3 years post-op. Kay’s repair is easy and cost effective for functional TR. Functional TR if moderate to severe should have annuloplasty irrespective of technique. There was no statistically significant difference in residual significant TR when comparing prosthetic ring with the De Vega SA. Both techniques significantly uplifted NYHA status. Bhagwan et al. (16) compared de Vega with prosthetic RA in functional TR in rheumatic population and found no statistically significant difference in residual significant TR and other echocardiographic parameters.
The highlight of our study is that we compared the combined techniques of SA (Kay’s and De Vega’s) with prosthetic RA in terms of the trends of certain selected echocardiographic parameters and grades of severity of TR in due course, that is pre/ post-op and follow up. The observation is that in both groups similar trends are recorded - fall in LVEF/ fall in RVSP and fall in TR Gmax. However, performance in RA group is better in terms of preserving LVEF, reduction of RVSP and reduction of TR Gmax. The last two parameters indicate trend towards reduction of pulmonary hypertension post TV repair. Finally, we say that there is no statistically significant difference between the parameters affection by both types of annuloplasty techniques (suture and ring). The trends of three parameters measured are statistically significant but the differences in parameters between both the groups are statistically non-significant. Ring annuloplasty appears to have performed shade better for these trends (Fig. 4).
On comparing both the groups we can say that the conversion of severe TR in pre-op to mild/ moderate in post-op and follow-up periods was achieved in both groups. However, RA performed better in achieving these results. In literature, the important aspects of RA, which makes it a better performer than SA are lower recurrence rate, more durable repair, greater long term stability and effective for severe cases.
|
Table 5. Explanations of how ring annuloplasty performed better |
|||
|---|---|---|---|
|
Parameter |
Suture Annuloplasty |
Ring Annuloplasty |
Interpretation |
|
Preoperative TR severity |
Similar (mostly severe TR) |
Similar |
Baseline comparable |
|
Postoperative mild TR (%) |
71.43 |
82.86 |
Ring shows higher immediate improvement |
|
Follow-up mild TR (%) |
68.57 |
82.86 |
Ring maintains better long-term mild TR |
|
Follow-up severe TR (%) |
11.43 |
5.71 |
Slightly fewer severe recurrences in ring group |
|
Trend over time |
Minor progression from mild→moderate |
More stable |
Ring annuloplasty offers more durable correction |
Significant differences in severity of TR favors RA in maintaining lower TR grades. Based on observed proportions, the ring group shows superior sustained improvement with less progression to moderate/severe TR. Both SA and RA effectively reduced TR severity immediately after surgery. RA demonstrated superior and more durable results, maintaining higher rates of mild TR and fewer recurrences of moderate/severe regurgitation at follow-up.
SA, although effective, showed slightly more late deterioration, possibly due to annular dilation recurrence. Both SA and RA resulted in significant reduction of TR severity postoperatively (p<0.001). At follow-up, mild TR was observed in 68.6% of patients with SA and 82.9% with RA.
Recurrence of moderate-to-severe TR was lower in the ring group (17.1%) compared to the suture group (31.4%). These findings suggest that RA provides more durable correction of TR than SA (Table 5).
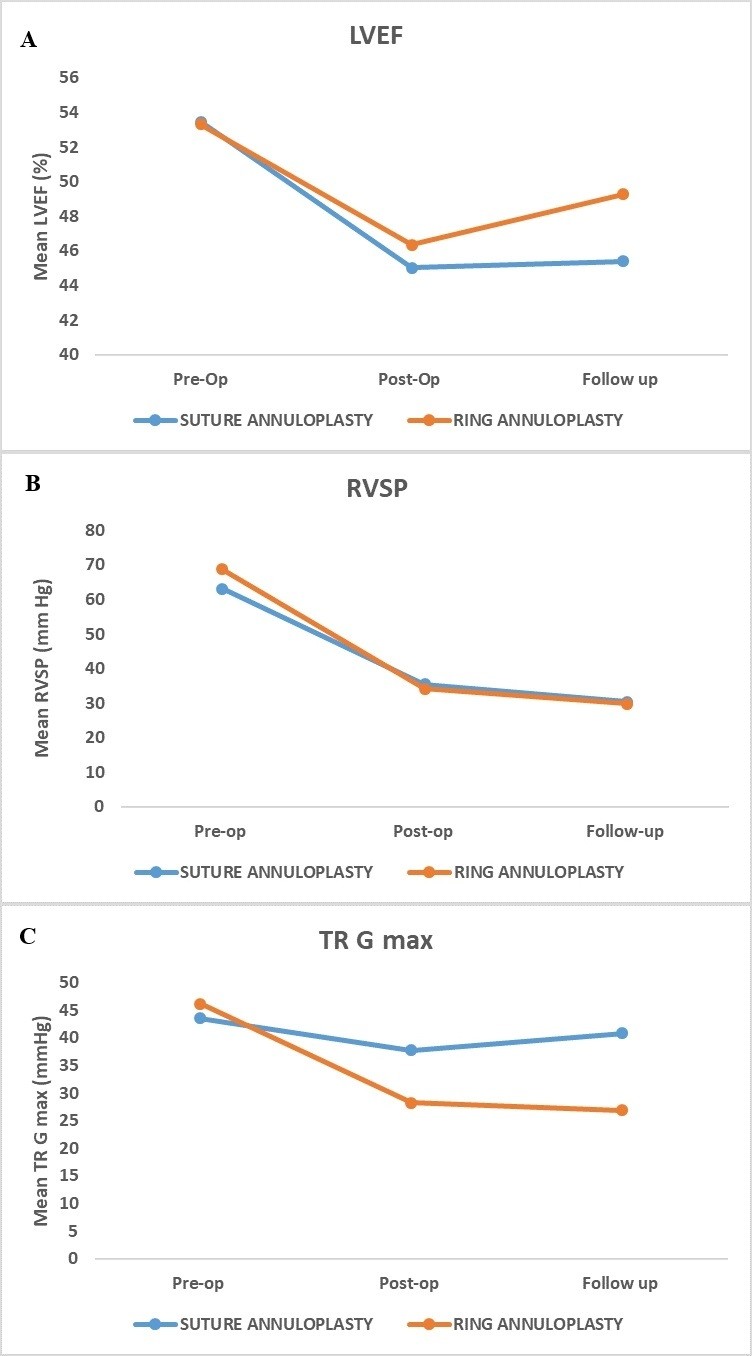
Figure 4. Trends of Echocardiographic Parameters (a- LVEF/ b- RVSP/ c- TAPSE)
LVEF- left ventricular ejection fraction, pre-op- preoperative, post-op – postoperative, RVSP -right ventricular systolic pressure, TR – tricuspid regurgitation, TR G max - maximal tricuspid regurgitation gradient
Study limitations
Also, we want to underline some limitations of the study for instance LVEF could be overestimated in case of regurgitant lesions. For mitral regurgitation it does not only reflect the blood volume pumped into the aorta, but also that is pumped into the low-pressure left atrium. Net aortic stroke volume is not actually calculated because a portion of the estimated pumped blood still remains in left ventricle. This in turn overestimates the LVEF (17).
The study is single institute study conducted in a tertiary set-up, still the authors believe that there can be limitations in terms of surgical techniques of valve replacement, types of prosthesis selected and difference in post-op ICU care. The authors acknowledge the continuation of further research on the topic.
Conclusion
We conclude that in both annuloplasty groups (suture and ring) there was a statistically significant affection in echocardiographic parameters, which was recorded with reference to pre-op values. However, on comparing both the groups (suture annuloplasty vs ring annuloplasty) the difference in both the groups was statistically non-significant with RA group performing shade better. The percentage of severe TR in pre-op as compared to post-p and follow-up periods reduced statistically significantly in both the groups. However, absolute reduction was more in RA group.
Hence, we conclude that both the techniques can be used with equal efficacy in terms of trends of echocardiographic parameters observed at pre-op/ post-op and follow-up periods with better correction of TR and performance in ring annuloplasty group.
Ethics: As this being a retrospective analysis of the surgical outcomes of the surgical technique, prior Ethics Committee approval was not taken. All the patients had consented for the surgery and our study being a retrospective study we have a waiver of individual consent of patient according to Institutional Ethics Committee.
Peer--review: External and internal
Conflict of interest: None to declare
Authorship: S.M. -conceptualization and study design, data acquisition, draft; A.P. - conceptualization and study design; S.K.T.R.- literature review; P.S. - statistics analysis, assistance in manuscript drafting, formatting, and coordination of the submission process. All authors critically review article and approved it for submission thus fulfilled all authorship criteria.
Acknowledgements and Funding: None to declare
Statement on A.I.-assisted technologies use: Authors declare that, Open AI product
Chat GPT 4.0 was used in the generation of ideas on statistical analysis but authors take
responsibility for whole manuscript writing process.
Data and material availability: Contact authors. Any share should in frame of fair use with acknowledgement of source and/or collaboration.
References
| 1.Condello F, Gitto M, Stefanini GG. Etiology, epidemiology, pathophysiology and management of tricuspid regurgitation: an overview. Rev Cardiovasc Med 2021; 22: 1115-42. https://doi.org/10.31083/j.rcm2204122 PMid:34957757 |
||||
| 2.Mahboobi SK, Sharma S, Ahmed AA. Tricuspid valve repair. In Stat Pearls [Internet] 2025 Jan 19. StatPearls Publishing. | ||||
| 3.Mulla S, Asuka E, Bora V, Sharma S, Siddiqui WJ. Tricuspid regurgitation. In StatPearls [Internet] 2024 Oct 6. StatPearls Publishing. | ||||
| 4.Caldas MM, Esteves WA, Nascimento BR, Hung J, Levine R, Silva VR, et al. Clinical outcomes and progression rate of tricuspid regurgitation in patients with rheumatic mitral valve disease. Open Heart 2023; 10: e002295. https://doi.org/10.1136/openhrt-2023-002295 PMid:37657848 PMCid:PMC10476137 |
||||
| 5.Hahn RT, Badano LP, Bartko PE, Muraru D, Maisano F, Zamorano JL, Donal E. Tricuspid regurgitation: recent advances in understanding pathophysiology, severity grading and outcome. Eur Heart J - Cardiovasc Imag 2022; 23: 913-29. https://doi.org/10.1093/ehjci/jeac009 PMid:35157070 |
||||
| 6.Unger P, Pibarot P, Tribouilloy C, Lancellotti P, Maisano F, Iung B, et al. European Society of Cardiology Council on Valvular Heart Disease. Multiple and mixed valvular heart diseases: pathophysiology, imaging, and management. Circulation: Cardiovasc Imag 2018; 11: e007862. https://doi.org/10.1161/CIRCIMAGING.118.007862 PMid:30354497 |
||||
| 7.Dreyfus GD, Corbi PJ, Chan KJ, Bahrami T. Secondary tricuspid regurgitation or dilatation: which should be the criteria for surgical repair? Ann Thorac Surg 2005; 79: 127-32. https://doi.org/10.1016/j.athoracsur.2004.06.057 PMid:15620928 |
||||
| 8.Tang GH, David TE, Singh SK, Maganti MD, Armstrong S, Borger MA. Tricuspid valve repair with an annuloplasty ring results in improved long-term outcomes. Circulation 2006; 114(1_suppl): I-577. https://doi.org/10.1161/CIRCULATIONAHA.105.001263 |
||||
| 9.Shinn SH, Dayan V, Schaff HV, Dearani JA, Joyce LD, Lahr B, et al. Outcomes of ring versus suture annuloplasty for tricuspid valve repair in patients undergoing mitral valve surgery. J Thorac Cardiovasc Surg 2016; 152: 406-15. https://doi.org/10.1016/j.jtcvs.2016.04.068 PMid:27260957 |
||||
| 10.Kisho M, Sarawy E, Abdelateif W. Kay annuloplasty of the tricuspid valve versus ring annuloplasty for repair of functional tricuspid regurgitation. JMed Sci Res 2020; 3: 190. https://doi.org/10.4103/JMISR.JMISR_79_19 |
||||
| 11.Belluschi I, Del Forno B, Lapenna E, Nisi T, Iaci G, Ferrara D, et al. Surgical techniques for tricuspid valve disease. Front Cardiovasc Med 2018;5: 118. https://doi.org/10.3389/fcvm.2018.00118 PMid:30234129 PMCid:PMC6127626 |
||||
| 12.Kosaraju A, Goyal A, Grigorova Y, Makaryus AN. Left ventricular ejection fraction. | ||||
| 13.Kotrri G, Youngson E, Fine NM, Howlett JG, Lyons K, Paterson DI, et al. Right ventricular systolic pressure trajectory as a predictor of hospitalization and mortality in patients with chronic heart failure. CJC open 2023; 5: 671-9. https://doi.org/10.1016/j.cjco.2023.05.011 PMid:37744660 PMCid:PMC10516718 |
||||
| 14.Aessopos A, Farmakis D, Taktikou H, Loukopoulos D. Doppler-determined peak systolic tricuspid pressure gradient in persons with normal pulmonary function and tricuspid regurgitation. J Am Soc Echocardiogr 2000; 13: 645-9. https://doi.org/10.1067/mje.2000.104535 PMid:10887347 |
||||
| 15.Türkmen U, Bozkurt T, Özyalçın S, Günaydın I, Kaplan S. Tricuspid repair: short and long-term results of suture annuloplasty techniques and rigid and flexible ring annuloplasty techniques. J Cardiothor Surg 2024; 19: 158. https://doi.org/10.1186/s13019-024-02640-y PMid:38539222 PMCid:PMC10967185 |
||||
| 16.Bhagwan J, Guha S, Gupta A, Padhy AK, Grover V, Gupta VK. A comparative analysis between ring annuloplasty and de Vega annuloplasty in functional tricuspid regurgitation. Int Surg J 2018; 5: 2131-6. https://doi.org/10.18203/2349-2902.isj20181975 |
||||
| 17.Yousef HA, Hamdan AE, Elminshawy A, Mohammed NA, Ibrahim AS. Corrected calculation of the overestimated ejection fraction in valvular heart disease by phase-contrast cardiac magnetic resonance imaging for better prediction of patient morbidity. Egypt J Radiol Nucl Med 2020; 51: 11. https://doi.org/10.1186/s43055-019-0130-8 |
||||
Authors` profile:
Shobhit Mathur - Assistant Professor, Department of Cardiovascular and Thoracic surgery, U.N. Mehta Institute of Cardiology and Research Center, Ahmadabad, Gujarat, India
Archit Patel - Associate Professor, Department of Cardiovascular and Thoracic surgery, U.N. Mehta Institute of Cardiology and Research Center, Ahmadabad, Gujarat, India
Sunil Kumar T. - Assistant Professor, Department of Cardiovascular and Thoracic surgery, U.N. Mehta Institute of Cardiology and Research Center, Ahmadabad, Gujarat, India
Pratik Shah - Research Officer, Department of Cardiovascular and Thoracic surgery, U.N. Mehta Institute of Cardiology and Research Center, Ahmadabad, Gujarat, India
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

