The right ventricle in pulmonary embolism – respect, never neglect
EDITORIALS
The right ventricle in pulmonary embolism – respect, never neglect
Article Summary
- DOI: 10.24969/hvt.2026.625
- CARDIOVASCULAR DISEASES
- Published: 31/01/2026
- Received: 19/01/2026
- Accepted: 19/01/2026
- Views: 263
- Downloads: 148
- Keywords: Pulmonary embolism, right ventricle, intervention
Address for Correspondence: Vitaliy Petrov, Department of Surgery, Cardiovascular Surgery and Transplantology, Danylo Halytsky Lviv National Medical University, Lviv, Ukraine
E-mail: vtly.12@gmail.com
ORCID: 0000-0002-2205-5403
Editorial
The right ventricle in pulmonary embolism – respect, never neglect
Vitaliy Petrov
Department of Surgery, Cardiovascular Surgery and Transplantology, Danylo Halytsky Lviv National Medical University, Lviv, Ukraine
Graphical abstract
Key words: Pulmonary embolism, right ventricle, intervention
Pulmonary embolism (PE) is a notorious life-threatening condition. It is currently the third most common cardiovascular cause of death worldwide, after myocardial infarction and stroke (1). Recognized as an entity two hundred years ago, it will very likely continue to retain its grim statistics for centuries to come.
The sudden appearance of thrombi in the pulmonary arteries inevitebly leads to reduced patency. When the internal diameter is reduced by half or more, the right ventricle (RV) afterload increases significantly. As a result, the RV may fail to tolerate it and eventually exhibits reduced contractility. It was firmly established at least as early as the ICOPER pulmonary embolism study (1999) that the key to understanding PE-associated mortality lies in the RV dysfunction (2).
ICOPER study (1999) showed that patients with a low RV ejection fraction had significantly worse survival than those with preserved RV function (2). This finding is now a cornerstone of contemporary PE understanding. While hypotension and obstructive shock are clear emergencies, even in hemodynamically stable patients RV contractility dictates the management strategy: decreased RV function prompts to desobstruct the pulmonary arteries as soon as possible.
It is noteworthy that the outcome frequently depends not the size or “mass” of the emboli, but on the RV the physiology.
Thrombotic material that does not appear “impressive” on CT imaging may still cause pronounced RV dysfunction. What makes the RV so uniquely vulnerable to a sudden increase in afterload? Some answers can be obtained with the help of three-dimensional (3D) imaging technologies.
Modern 3D medical reconstructions of the heart allow clear visualization of the structural differences between the right and left ventricles (LV). Notably, 3D models demonstrate that the RV is actually located anteriorly rather than on the “right,” while the LV is positioned posteriorly rather than on the “left” (3) – a relationship crucial for understanding the images that follow.
At least two features of the ventricles can be highlighted: mass and shape.
Figure 1 shows that the RV anterior wall measures approximately 3 mm, while the LV walls are about three times thicker. This discrepancy evidently contributes to the significant difference in force generation and the ability to withstand elevated afterload.
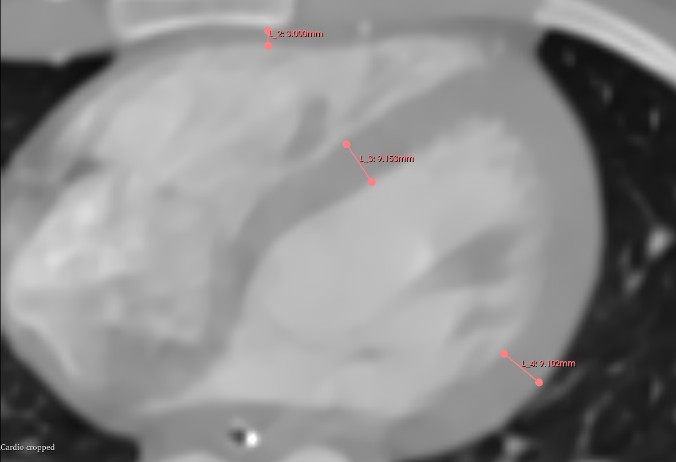
Figure 1. Computer tomography scan of a normal heart
Figure 2 demonstrates that the normal LV resembles an ellipsoid or a cone, while the RV does not share this geometry. It has been shown that the unique LV shape allows for favorable intracavitary stress distribution (4).
Figure 3 illustrates how the RV is located on the anterior surface of the LV, almost as if superimposed. Its posterior wall—the interventricular septum—is concave toward the RV chamber, while the anterior wall (the anterior cardiac surface) is convex. Thus, the RV does not share the stress distribution patterns described for the LV.
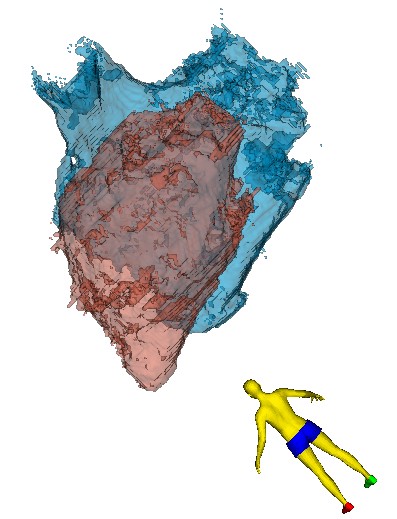
Figure 2. 3D reconstruction of the LV and RV as seen from the left postero-cranial view (back of the heart)
3D – 3- dimensional, LV- left ventricle, RV – right ventricle
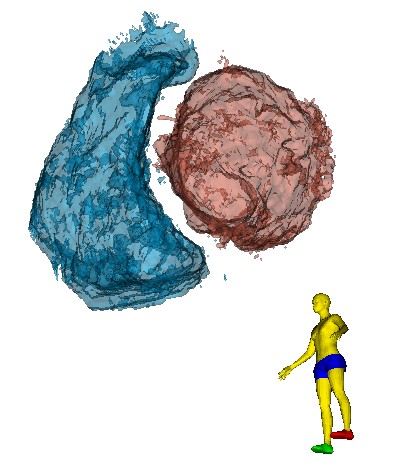
Figure 3. 3D reconstruction of the RV and LV as seen from the left caudal view (apex of the heart)
3D – 3- dimensional, LV- left ventricle, RV – right ventricle
With these considerations in mind, we read with interest the recent report by Sanchez Cortes et al. (5) who described a challenging case of PE in a postpartum lady. The authors clearly demonstrated RV dilatation accompanied by reduced contractility—one of the most important signs of imminent deterioration. Thus, a timely decision to des-obstruct the pulmonary arteries was made, and because of strong contraindications to thrombolysis, endovascular aspiration was performed.
Currently, three strategies are available for the treatment of high‑risk PE: open-heart surgery, thrombolysis, and endovascular aspiration. Their use is primarily determined by patient‑specific contraindications and the availability of resources within a healthcare facility. However, the risk of mortality is dictated primarily by the RV—the maxime magni momenti of PE.
Peer-review: Internal
Conflict of interest: None to declare
Authorship: V.P.
Acknowledgements and Funding: None to declare.
Statement on A.I.-assisted technologies use: Author stated they did not use artificial intelligence (A.I.) tools for writing manuscript
Data and material availability: Does not apply
References
| 1.Martin SS, Aday AW, Allen NB, Almarzoog ZI, Anderson CAM, Arora P, et al. 2025 Heart and Stroke statistics report. Circulation 2025; 151: doi: 10 1161/CIR.0000000000001309 https://doi.org/10.1161/CIR.0000000000001303 |
||||
| 2.Goldhaber SZ, Visani L, De Rosa M. Acute pulmonary embolism: Clinical outcomes in the International Cooperative Pulmonary Embolism Registry (ICOPER). Lancet 1999; 353: 1386-9. Doi: 10.1016/S0140-6736(98)07534-5 https://doi.org/10.1016/S0140-6736(98)07534-5 PMid:10227218 |
||||
| 3.Petrov V. Comment on "Left ventricular perforation by a chest tube: Case report and review of complications". Mind the left ventricle posterolateral wall please! Heart Vessels Transplant 2024; 8: 160-2. doi.org/10.24969/HVT.2024.461 https://doi.org/10.24969/hvt.2024.461 |
||||
| 4.Zhong L, Ghista DN, Tan RS. Left ventricular wall stress compendium. Comp Meth Biomech Biomed Engin 2012; 15; 1015-41. doi.org/10.1080/10255842.2011.569885 https://doi.org/10.1080/10255842.2011.569885 PMid:21547783 |
||||
| 5. Sanchez Cortes E, Valencia Gonzalez JD, Guzman Olea J, Franquez Flores EJ, Cruz Palomera R, Miguel Salvador AR. The birth of a thrombus: Pulmonary embolism during the puerperium treated with percutaneous thrombectomy- a case report. Heart Vessels Transplant 2026; 10: XXX-XX. | ||||
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

