What's new in the updated American Society of Echocardiography guidelines for ultrasound-guided vascular cannulation?
EDITORIALS
What's new in the updated American Society of Echocardiography guidelines for ultrasound-guided vascular cannulation?
Article Summary
- DOI: 10.24969/hvt.2025.579
- CARDIOVASCULAR DISEASES
- Published: 14/07/2025
- Received: 12/07/2025
- Accepted: 12/07/2025
- Views: 2931
- Downloads: 1653
- Keywords: Ultrasonography, vascular, cannulation, guidance, veins, arteries, guidelines
Address for Correspondence: Kairgeldy Aikimbaev, Radiology Department, Medical Faculty, Cukurova University, Adana, Turkiye
Email: aikimbaev@gmail.com
ORCID: 0000-0002-5436-6492
What's new in the updated American Society of Echocardiography guidelines for ultrasound-guided vascular cannulation?
Kairgeldy Aikimbaev
Radiology Department, Medical Faculty, Cukurova University, Adana, Turkiye
Key words: Ultrasonography, vascular, cannulation, guidance, veins, arteries, guidelines
Vascular cannulation is a fundamental yet challenging minimally invasive procedure in clinical practice frequently performed to facilitate patient care due to its proven direct access to the circulation for administering medications, hemodynamic monitoring, and critical care support. Vascular access includes (a) peripheral vein cannulation, a basic technique and skill required in difficult cases, such as a young child with thin veins, the elderly with fragile veins, the extremely obese, and when all major veins are already occluded due to preexisting conditions and complications, (b) central venous catheters, and (c) arterial access.
Additional challenging situations that may lead to adverse events occur more often with less experienced operators, challenging patient anatomy due to congenital anomalies such as persistent left superior vena cava, compromised procedural settings (emergency or mechanical ventilation), and the presence of severe comorbidities such as coagulopathy and emphysema (1).
Vascular cannulations under direct vision (superficial vessel, through cut-down) or landmark orientation are among the old-style techniques in terms of history. Traditional landmark-based techniques rely on anatomical cues and palpation, which can be unreliable in patients with obesity, hypovolemia, or aberrant anatomy, leading to increased complications. The introduction of ultrasound-guided vascular cannulation (UGVC) has revolutionized this practice by enabling real-time visualization of vessels, significantly improving success rates and patient safety. Multiple studies and meta-analyses have demonstrated that UGVC reduces the number of attempts, decreases complications, and shortens procedure time compared to landmark orientation techniques (2-6). For central venous catheterization, ultrasound guidance is now considered the gold standard, as endorsed by the American Society of Anesthesiologists and the National Institute for Health and Care Excellence, due to its proven reduction in carotid artery punctures and pneumothorax (7). Similarly, in peripheral venous access, UGVC has become indispensable for difficult-to-cannulate patients, reducing reliance on central lines and improving resource utilization (8).
Despite its clear advantages, UGVC remains underutilized in many settings due to barriers such as lack of training, equipment availability, and time constraints. To address these challenges, the American Society of Echocardiography recently published UGVC recommendations (9), constructed on evidence-based data and the up-to-date literature, replacing previous recommendations published 14 years ago (7).
The purpose of this Editorial is to briefly outline the main innovations and significant differences between the current recommendations and the previous ones.
1.Methodology and Evidence Review
2011 edition: A comprehensive search of English-language articles using PubMed and MEDLINE databases was conducted for original research studies on ultrasound-guided vascular access published in peer-reviewed scientific journals between 1990 and 2011. While scientific evidence regarding the strength of the recommendation was assessed in subjective categories (A = supportive, B = suggestive, C = uncertain, and D = insufficient), only category A evidence was accepted for recommendations (7).
2025 update: By searching the same databases with a similar approach, articles published between 1990 and 2023 were included in the analysis. The Grading of Recommendations Assessment Development and Evaluation system (10) to assess the evidence levels and base the recommendation grade was chosen, and only strong evidences were accepted for recommendations (9).
2. Anatomical Coverage
2011 edition: Focused primarily on central venous cannulation (internal jugular, subclavian, femoral veins), with additional sections on arterial and pediatric access, and comparing real-time versus static ultrasound use (7).
2025 update: Extensively expanded to include both central and peripheral venous and arterial access across adult and pediatric populations, covering radial, ulnar, brachial, axillary, carotid, femoral, posterior tibial, and dorsalis pedis arteries (9).
3. Technical Focus and Key Role Clarification
2011 edition: Emphasized choosing between real-time versus static ultrasound imaging, and fundamentals of probe orientation and needle guidance (7).
2025 update: Clearly delineates three essential clinical functions of ultrasound in cannulation: pre‑cannulation vessel assessment, dynamic real‑time guidance during cannulation, and post‑cannulation detection of complications. The update also integrates detailed diagrams, ultrasound images, and videos to support these functions (9).
4. Expanded Vascular Sites and Subspecialty Detail
2011 edition: Covered main central sites; arterial and peripheral venous access received limited coverage (7).
2025 update: Adds peripheral venous cannulation and detailed arterial techniques for all major limb vessels and carotids, plus pediatric-specific sections ensuring comprehensive guidance in diverse clinical contexts (9).
5. Complications and Training Emphasis
2011 edition: Touches on complications and training/simulation basics (7).
2025 update: Provides an in-depth nomenclature of local and arterial complications (hematoma, thrombosis, nerve injury, pseudoaneurysm, arteriovenous fistula, etc.), as well as detailed pediatric complication management, plus standardized training curricula and competency assessments (9).
6. Evidence Gaps and Future Directions
2011 edition: Noted varying evidence levels, with some recommendations based on limited data (7).
2025 update: Acknowledges persistent evidence gaps and explicitly states accessibility (operator skill/ultrasound availability) will likely determine practice adoption more than future studies (9).
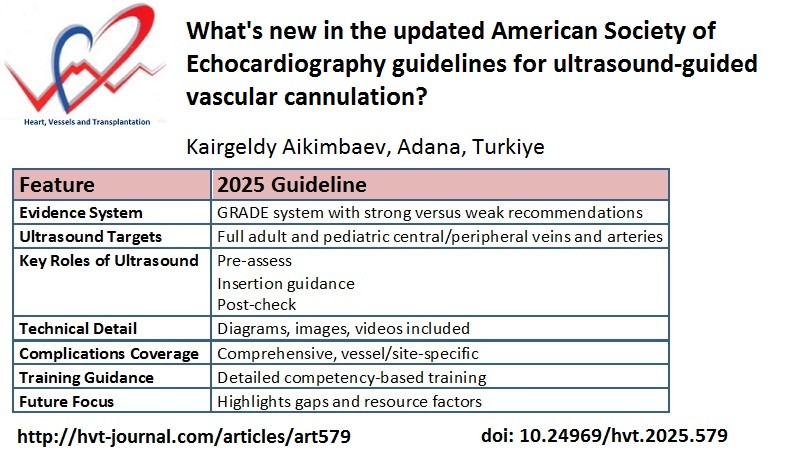
The summary of the main innovations and significant differences between the current recommendations and the previous ones presented in the Table 1.
|
Table 1. Principle differences between previous and updated guidelines for ultrasound-guided vascular cannulation from American Society of Echocardiography (7, 9) |
||
|
Feature |
2011 Guideline |
2025 Guideline |
|
Evidence System |
Category A-D |
GRADE system with strong versus weak recommendations |
|
Ultrasound Targets |
Mainly central veins; basic arterial |
Full adult and pediatric central/peripheral veins and arteries |
|
Key Roles of ultrasound |
Real-time vs static imaging |
Pre-assess Insertion guidance Post-check |
|
Technical Detail |
Probe orientation, basics |
Diagrams, images, videos included |
|
Complications Coverage |
Overview |
Comprehensive, vessel/site-specific |
|
Training Guidance |
Broad recommendations |
Detailed competency-based training |
|
Future Focus |
Limited |
Highlights gaps and resource factors |
Conclusions
The 2025 updated American Society of Echocardiography guideline marks a significant leap in breadth and depth: upgraded evidence grading, expanded anatomical coverage, systematic breakdown of ultrasound roles, and robust training and complication frameworks. It reflects a decade of technological advancement, increased clinical use, and a nuanced understanding of ultrasound’s role in safe vascular access.
Peer-review: Internal
Conflict-of-interest: None to declare
Author contributions: K.A.
Acknowledgement and Funding: None to declare
Statement on A.I.-assisted technologies use: Author declare that they did not use AI-assisted technologies in preparation of this manuscript
Availability of data and material: Do not apply
References
| 1.Bodenham A. Vascular access. Rev Med Clin Condes 2017: 28: 701-12. doi: 10.1016/j.rmclc.2017.07.011 https://doi.org/10.1016/j.rmclc.2017.07.011 |
||||
| 2.Hind D, Calvert N, McWilliams R, Davidson A, Paisley S, Beverley C, et al. Ultrasonic locating devices for central venous cannulation: meta-analysis. BMJ 2003; 327: 361. doi: 10.1136/bmj.327.7411.361 https://doi.org/10.1136/bmj.327.7411.361 PMid:12919984 PMCid:PMC175809 |
||||
| 3.Brass P, Helmich M, Kolodziej L, Schick G, Smith AF, Cochrane Emergency and Critical Care Group. Ultrasound guidance versus anatomical landmarks for internal jugular vein catheterization. Cochrane Database Syst Rev 2015; 1: CD006962. doi: 10.1002/14651858.CD006962.pub2 https://doi.org/10.1002/14651858.CD006962.pub2 PMid:25575244 PMCid:PMC6517109 |
||||
| 4.Flumignan RL, Trevisani VFM, Lopes RD, Baptista-Silva JCC, Flumignan CDQ, Nakano LCU. Ultrasound guidance for arterial (other than femoral) catheterisation in adults. Cochrane Database Syst Rev 2021; 10: CD013585. doi: 10.1002/14651858.CD013585.pub2 https://doi.org/10.1002/14651858.CD013585.pub2 PMid:34637140 PMCid:PMC8507521 |
||||
| 5.Tada M, Yamada N, Matsumoto T, Takeda C, Furukawa TA, Watanabe N. Ultrasound guidance versus landmark method for peripheral venous cannulation in adults. Cochrane Database Syst Rev 2022; 12: CD013434. doi: 10.1002/14651858.CD013434.pub2 https://doi.org/10.1002/14651858.CD013434.pub2 PMid:36507736 PMCid:PMC9744071 |
||||
| 6.Singhal MK, Virendra K, Misra S, Das PK, Giri M, Chaudhary S. A comparative study of conventional versus ultrasound-assisted femoral arterial cannulation: a prospective randomized trial. Cureus 2025; 17: e80871. doi: 10.7759/cureus.80871 https://doi.org/10.7759/cureus.80871 |
||||
| 7.Troianos CA, Hartman GS, Glas KE, Skubas NJ, Eberhardt RT, Walker JD, et al. Guidelines for performing ultrasound guided vascular cannulation: recommendations of the American Society of Echocardiography and the Society of Cardiovascular Anesthesiologists. J Am Soc Echocardiogr 2011; 24: 1291-318. doi: 10.1016/j.echo.2011.09.021 https://doi.org/10.1016/j.echo.2011.09.021 PMid:22115322 |
||||
| 8.Fields JM, Piela NE, Au AK, Ku BS. Risk factors associated with difficult venous access in adult ED patients. Am J Emerg Med 2014; 32: 1179-82. doi: 10.1016/j.ajem.2014.07.008 https://doi.org/10.1016/j.ajem.2014.07.008 PMid:25171796 |
||||
| 9.Vegas A, Wells B, Braum P, Denault A, Miller Hance WC, Kaufman C, et al. Guidelines for Performing Ultrasound-Guided Vascular Cannulation: Recommendations of the American Society of Echocardiography. J Am Soc Echocardiogr 2025; 38: 57-91. doi: 10.1016/j.echo.2024.12.004 https://doi.org/10.1016/j.echo.2024.12.004 PMid:39909653 |
||||
| 10.Guyatt G, Gutterman D, Baumann MH, Addrizzo-Harris D, Hylek EM, Phillips B, et al. Grading strength of recommendations and quality of evidence in clinical guidelines: report from an American College of Chest Physicians Task Force. Chest 2006; 129: 174-81. doi: 10.1378/chest.129.1.174 https://doi.org/10.1378/chest.129.1.174 PMid:16424429 |
||||
Copyright

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
AUTHOR'S CORNER

